
Sinusitis Treatment
Patients with persistent or recurrent sinusitis who have not responded to medicinal interventions, therapies, or have a structural component contributing to their sinus blockage may benefit from surgery. Penn Medicine Becker ENT & Allergy Center in New Jersey and Pennsylvania provides sinus surgery as one of its services.
Most patients suffering with signs and symptoms of sinusitis find relief with medical treatments. Nasal steroids, nasal antihistamines, saline nasal irrigation, oral antihistamines, and oral anti-leukotrienes along with a vast supply of over-the-counter (OTC) medications are sufficient for most patients with sinus pressure, pain, congestion, smell disturbances, and headaches.
On occasion antibiotics and oral steroids may also be used to treat patients with recurrent sinus infections. For some patients; however, these medications are insufficient to provide long-term relief, and symptoms persist despite prolonged medical therapy. In instances where the sinus function is impeded as a result of structural blockage, surgery may be recommended as a way to remove the blockage and open the sinuses to restore natural drainage.

- What is sinusitis, and what causes it?
- Types of Sinusitis
- What are the indications of acute sinusitis?
- What are the signs associated with chronic sinusitis?
- Would you benefit from sinus relief?
- Anatomy of the Sinuses
- What over the counter medications can help me?
- The Benefits of Sinus Surgery (Functional Endoscopic Sinus Surgery)
- Why choose a sinus specialist?
- Who is a Candidate for a Sinus Surgery?
- When is it advisable to seek medical attention from a doctor?
- Your Sinus Surgery Consultation
- What is Functional Endoscopic Sinus Surgery (FESS) and how is it performed?
- Sinusitis FAQs
What is sinusitis, and what causes it?
Sinusitis (or technically Rhinosinusitis) refers to inflammation of the nose and sinuses. Contrary to popular belief, sinusitis is an inflammatory – not infectious – disease. While patients may get sinus infections, it is the underlying inflammation that sets the stage for an infection to occur.
There are a number of common causes of nasal irritation and inflammation, including allergens, non-allergic pollutants, cigarette smoke and viruses. These can often lead to obstruction of the osteomeatal complex (sinus drainage pathway) from mucosal swelling and this leads to secondary bacterial sinusitis, which causes additional inflammation.
In addition, anatomic abnormalities such as polyps, tumors, foreign bodies (especially in children), enlarged adenoids, deviated nasal septum, and aerated middle turbinates (concha bullosa), may cause initial obstruction with the same result. It is common to see more than one contributing factor.
Other factors that may contribute to sinonasal inflammation include hormonal reactions associated with pregnancy, aging, medication misuse, medication reactions, and acid reflux.
Types of Sinusitis
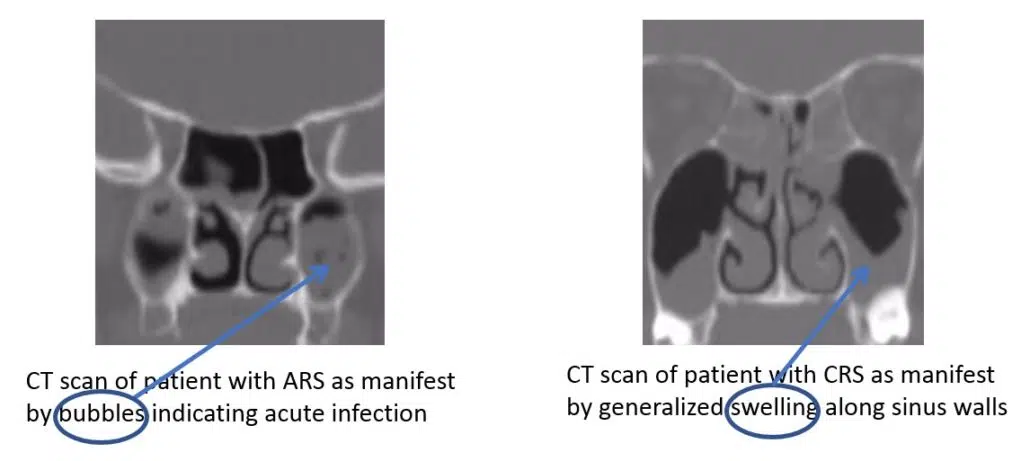
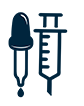
Sinusitis is typically classified as Acute or Chronic based on duration and symptomatology. In Acute Rhino-Sinusitis (ARS) – typically referred to as a “sinus infection” – patients experience purulent (discolored) nasal drainage along with nasal obstruction, facial pain, facial pressure, and/or facial fullness for up to 4 weeks. Patients with ARS may also experience cough, fever, fatigue, diminished sense of smell, dental pain and ear fullness – although these common symptoms are not required for diagnosis. In Chronic Rhino-Sinusitis (CRS), patients experience nasal obstruction, facial congestion/pressure/fullness, discolored nasal discharge, diminished sense of smell for over 12 weeks. Symptomology alone is insufficient for a diagnosis of CRS, as patients must also be found to have polyps, edema, thick discharge or discolored mucous on objective exam (usually either an in-office nasal endoscopy, or CT imaging). There is, of course, overlap and interplay between these diagnostic groups – patients with ARS may develop long-term symptoms that evolve into CRS, and patients with CRS may experience acute, infectious exacerbations.
What are the indications of acute sinusitis?
Acute sinusitis can last up to 4 weeks and may be viral or bacterial in origin. Recurrent sinusitis refers to the situation where a patient has repeated acute sinus infections but is relatively symptom free between these infections. Symptoms of acute sinusitis can include:
Post Nasal Drip and Cough
Nasal Blockage and Congestion
Sinus Pressure and Headache
Sinus Infections
Diminished Smell and Taste
It is common for patients to come to their Ear Nose and Throat physician (ENT) with a complaint of a post nasal drip (PND) sometimes associated with congestion and cough. It is sometimes difficult to identify the exact source of this PND; however, that does not mean it cannot be successfully treated. Similarly, it may be difficult to ascertain the exact relationship between PND and cough; however, a methodical and meticulous approach often leads to improvement or resolution of symptoms. After taking a thorough history and physical exam, your ENT physician may suggest a variety of treatment options including trials of prescription nasal sprays (ie-steroids, antihistamines, anticholinergics), oral allergy medications, saline irrigations, and some over-the-counter (OTC) medications such as Guafenesin. Often these treatments are successful. In cases where they are not, other tests – such as in-office Endoscopy, Allergy testing, Sinus CT, Chest XRay – may be ordered or performed to hone in on potential sources.
Nasal blockage or obstruction should be distinguished from nasal congestion which is a related and overlapping diagnosis. Nasal congestion is a sensation of “stuffiness” and is often due to swelling of the nasal and sinus lining. Patients with congestion often complain of repeatedly blowing their nose but “nothing comes out.” This is distinct from nasal obstruction which is the blockage or impediment of air to flow freely in and out of the nose. Often obstruction is caused by a structural blockage – deviated septum, enlarged turbinates, nasal mass or polyps, enlarged adenoids – and responds best to surgical intervention (ie-septoplasty, turbinate reduction, etc) when medications are ineffective. Congestion; however, is usually responsive to medical intervention. Patients with nasal obstruction may also have congestion and vice-versa. Effective treatment is dependent on accurate diagnosis.
When the sinus lining swells, the ostia become blocked, the mucous backs up and symptoms occur. Under these circumstances, patients often complain of facial pressure and sinus headaches. Sinus headaches should be differentiated from other types of headaches (ie-Migraines, Cluster, Tension headaches) and it is important to properly diagnose headache type so that effective and targeted treatment can be prescribed. Treatment of sinus pressure and headaches focuses on finding ways to take down nasal and sinus swelling in order to open blocked sinus ostia and re-establish natural sinus drainage.
As described above, sinuses drain through small openings or ostia which can be blocked by swollen lining (exacerbated by viral infection, allergies, etc) or structural components (deviated septum, polyps, scar tissue, etc). When sinuses are blocked, the mucous backs up and serves as a breeding ground for bacteria, sometimes leading to a sinus infection. For most uncomplicated acute sinusitis, treatment may begin with symptomatic therapy such as analgesics (ie-Acetaminophen, Ibuprofen), topical nasal corticosteroids (ie-Fluticasone, budesonide, triamcinolone, etc), and saline nasal irrigation. If symptoms persist or worsen, antibiotics may be prescribed. In some cases, a culture may be taken in the office using a small endoscope and a sinus swab to identify specific bacteria involved in the infection. This can help narrow down the diagnosis and identify the most effective antibiotic for treatment.
It is common for patients with ARS and CRS to complain of a diminished (hyposmia) or missing (anosmia) sense of smell and/or taste. Smell is transmitted via the 1 st (Olfactory) Cranial Nerve which is located at the top of the nasal/sinus cavity, and accounts for a large part of taste sensation as well. When the nose and sinus lining swells – as it does in acute and chronic sinusitis – the stream of odorants (substances containing molecules that trigger the smell nerves) – is blocked from reaching the receptors of the Olfactory Nerve, and patients experience a diminished sense of smell and taste. When a patient’s sinus condition resolves, the odorants are no longer obstructed and the sense of smell and taste often improves. There are other causes of diminished smell and taste – primary disorders of the olfactory nerve, brain tumors, nasal masses and polyps, viral infection, trauma, etc – each of which has its own treatment algorithm; however, for most patients with ARS and/or CRS, treatment focuses on taking down the inflammation associated with sinusitis.
Additional Symptoms:
- Fever, Fatigue, and/or Dental Pain
- Bad Breath
- Thick, Green or Yellow Nasal Discharge
- Respiratory infections
What are the signs associated with chronic sinusitis?
Chronic sinusitis sufferers may have the following symptoms for 12 weeks or more:
- Facial Pain/Pressure/Headaches Nasal Obstruction/Blockage
- Nasal Discharge/Discolored Post-Nasal Discharge
- Pus in the Nasal Cavity
- Diminished Sense of Smell
- Cough
- Stuffy nose.
Additional Symptoms:
- Headaches
- Fever, Fatigue, and/or Dental Pain
- Bad Breath

Would you benefit from sinus relief?
At Penn Medicine Becker ENT & Allergy, our New Jersey and Philadelphia Sinus specialists are highly-trained sinus experts who provide individualized treatment plans for patients who need help with their nose, allergies, and sinuses. We combine our experience and training with cutting-edge technology to be true Leaders in Sinus Relief.
Many treatment options are available for those who suffer from:
- Congestion
- Diminished Sense of Smell
- Facial Pain/Pressure/Headaches
- Cough & Post Nasal Drip
- Sinus Infection & Sinusitis
- Nasal Obstruction/Blockage
- Nasal Discharge

Medication
Nasal sprays and oral medications may provide partial or complete relief
Allergy Treatments
Allergy testing to show if you can benefit from allergy shots or drops

In-Office Procedures
New technologies allow for short, in-office procedures designed to address sinus -related symptoms

Sinus Surgery
With minimally-invasive oupatient surgery, patients can reclaim normal sinus function
Anatomy of the Sinuses
There are 4 chamber-like sinuses on each side of the face. These are named the Maxillary sinuses (below the eyes), Frontal sinuses (above the eyes), Ethmoid sinuses (between the eyes), and Sphenoid sinuses (all the way in the back). The Ethmoid sinuses may be divided into an anterior (front) and posterior (back) group. The sinuses drain through small openings – called “ostia” – into the nasal cavity. Mucous drains down the nasal cavity and into the throat from where it is swallowed into the esophagus and stomach.
Each sinus drains into a specified area. The maxillary, anterior ethmoid, and frontal sinuses all drain into the “middle meatus”. The drainage of the posterior ethmoid sinuses occurs in the “superior meatus,” while the sphenoid sinuses drain into the “spheno-ethmoidal recess.”
The sinuses are lined by a mucous-producing mucosa. The mucosa produces over one liter of mucous daily, so it is imperative that the drainage pathways remain clear and open. When the sinus lining swells – from allergies, irritants (dust, chemicals), infections – the drainage openings narrow, and mucous production increases leading to a back-up. If the situation persists it can lead to infection (acute rhinosinusitis) or long-term swelling and sinus dysfunction (chronic rhinosinusitis).
In situations where structural blockage is determined to be a significant causative factor of sinus blockage, inflammation, or infection, surgical correction may be recommended. Below please find descriptions of sinus surgery along with answers for associated frequently asked questions.
What over the counter medications can help me?
For patients suffering from sinus issues for fewer than 7 days, here is a list of some over the counter medications that can help alleviate symptoms:
- Mucinex (Guaifenesin)
- Tylenol Cold & Sinus
- Advil Cold & Sinus
- Sudafed
- Robitussin DM
- Claritin, Zyrtec or Allegra (Oral antihistamines)
As always, these medications must be used with care, and in accordance with recommended uses and precautions.
Topical decongestants are not recommended for chronic sinusitis. When topical decongestants are used for more than three to five days, a “rebound effect” with worsened symptoms will typically result.
Oral decongestants may raise blood pressure, and patients and their doctors should monitor blood pressure and may need to discontinue oral decongestants if blood pressure is affected. Oral decongestants may also impact other conditions such as prostate hypertrophy, and glaucoma, and the medication labels must be carefully adhered to.
Since higher concentrations are present in the bloodstream, systemic decongestants are more likely to produce side-effects. These include high blood pressure, anxiety and sleeplessness, and the “jitters.” Decongestants can also cause blurry vision (in patients who suffer from glaucoma) and difficulty urinating in patients with prostate problems.
Patients should let their doctor know if they are currently taking any medications for depression, since these medications can have serious adverse effects when they interact with either topical or systemic decongestants. Mucolytics, Antifungals and Macrolides, and others.
Schedule your consultation
The Benefits of Sinus Surgery (Functional Endoscopic Sinus Surgery)
Patients who suffer from persistent or recurrent signs and symptoms of sinusitis which have not responded to medical interventions and therapies, and who have a structural component contributing to their sinus blockage may benefit from surgical intervention. Patients typically report significant improvement in their sinus-related symptoms after surgery. This includes decrease in sinus-related facial pressure, congestion, nasal obstruction, rhinorrhea, and headache. Multiple studies support improvement in patient-reported quality of life measures, as well as objective findings on nasal endoscopy and CT scans. Published data demonstrates that even patients with other factors (co-morbidities) which might impact outcomes – asthma, smoking, allergies, prior sinus surgery – experience significant improvement after sinus surgery. In some cases, patients may still need medications (ie-nasal steroid sprays, nasal anti-histamines, saline irrigations, etc) to treat and manage the underlying disease process (sinusitis); however, unlike before surgery the medications are typically more effective since the sinuses will be open and accessible to topical medicines.
Why choose a sinus specialist?
Many people live with sinus-related issues and don’t realize that effective treatment is available. While you have the option to use over-the-counter medications to help ease your symptoms, you may find greater relief if you can identify and methodically treat the underlying source of your problem. A quick but thorough evaluation is the starting point for a comprehensive treatment plan to provide maximum, sustained relief for your nose, sinus and allergy-related symptoms. Patients are often surprised to learn that what has become a normal way of living can be relieved through something as simple as allergy treatment, or a mild in-office procedure like Balloon Sinuplasty.
Without a thorough evaluation, it is impossible to understand exactly what is causing your sinus-related issues. Schedule an appointment with a sinus specialist, and ask about allergy testing if you have not recently been tested.
Who is a Candidate for a Sinus Surgery?
Your physician will typically look for the least invasive means to help you manage your sinusitis symptoms and decrease the impact of sinus inflammation on your quality of life. In most cases, this will involve a series of medical treatments such as prescribed and over-the-counter oral pills, topical sprays, and irrigations. Ancillary tests – CT scans, allergy testing, etc – may be ordered to identify the root cause of your sinus swelling. In cases where medications do not provide sufficient, sustainable, long-term relief, and where there is felt to be a structural component to the sinus blockage, surgery may be considered. Opening the small sinus ostia is performed as a means to restore natural sinus drainage and to allow the sinus lining to return to its normal, healthy state.
When is it advisable to seek medical attention from a doctor?
If you are suffering from a cold for more than 10 days, or if your symptoms worsen after the first 7 days, you should consider seeing a sinus specialist. Many sinus doctors reserve spots for same-day appointments to accommodate sick patients. If you are not feeling better 3 to 5 days after starting antibiotics for a sinus infection, you should let your prescribing physician know.
Your Sinus Surgery Consultation
A visit to your New Jersey or Philadelphia or Yardley ENT doctor will include a thorough review of your symptoms, as well as a history of any medications and other treatments that you have tried in the past. Your physician will look for medications that you have not tried, or perhaps medications you have tried that may be worth trying again in combination with other treatments. A focused exam – typically including a brief nasal endoscopy – will be performed to assess the status of the nose and sinus anatomy, and to identify any obvious abnormalities that might be contributing to your sinus condition. Prior testing will be reviewed, and further testing may be ordered. Once a complete assessment has been performed, a treatment plan will be developed and reviewed with you. This may include surgery, or perhaps an additional trial of medications to see if success can be achieved without surgery. If you decide with your physician that surgery such as endoscopic sinus surgery is an appropriate next step, details about the particular procedures to be performed will be discussed, and any and all questions answered.
What is Functional Endoscopic Sinus Surgery (FESS) and how is it performed?
FESS is surgery designed to open blocked sinuses and restore natural drainage pathways. The past decade has seen significant evolution in the surgery, so that it is now typically performed as a minimally-invasive, outpatient procedure. Small (4mm) endoscopes are placed in a patient’s nostrils to access and visualize the sinuses. These endoscopes are available with a variety of angled lenses to allow maximal visualization of the sinuses. Using specially designed surgical instruments the sinus ostia are identified and enlarged. Obstructing tissue and bone are carefully removed taking care to preserve the sinus lining which will usually return to its natural, healthy state once surgical healing is completed. In many cases, your surgeon will perform your sinus surgery using an Image Guidance Navigation System –a type of specialized GPS system which allows real-time tracking of surgical instrumentation in 3 dimensions. Also, dissolvable sutures are often used to keep the operated structures in place while they heal. Small absorbable spacers may also be placed for this purpose, as well as dissolvable implants which give off medications for several weeks to assist in the healing process. In addition, an ENT specialist will provide a guide to a successful recovery from sinus surgery.
Additional procedures besides Sinus Surgery
In some cases, additional anatomical structures may contribute to a patient’s symptoms and should be addressed in order to maximize outcomes. Septal deviation, enlarged turbinates, enlarged adenoids, concha bullosa are all adjacent structures that may impact a patient’s nose and sinus related health. If surgery on these structures is recommended, it can usually be performed during the same operation. Your surgeon will of course discuss what is most suitable for your particular situation.

Pick one of our convenient locations
for your Sinusitis Treatment

