
Thyroid Disease Treatment
Do you or a loved one suffer from thyroid disease? Penn Medicine Becker ENT & Allergy can help! With our top-notch ENT providers, we help to provide diagnosis and treatment for thyroid disorders. Whether it’s thyroid masses, thyroid nodules, or thyroid goiter, our experienced team is here to help. We work closely with our primary care and endocrinology colleagues and understand how difficult it can be to manage a thyroid disorder. We will work with you every step of the way to ensure your best possible health.
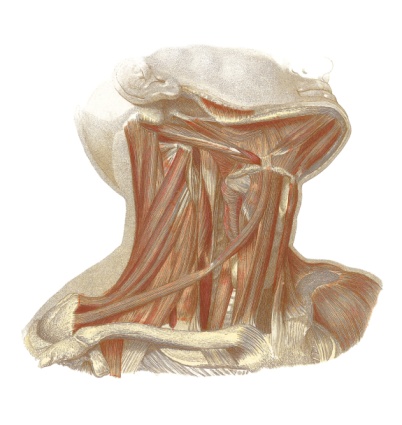
Understanding the Thyroid Gland
The thyroid gland, located at the base of the neck, plays a crucial role in regulating the body’s metabolism and energy levels. Its butterfly-shaped structure consists of two lobes connected by a narrow strip of tissue called the isthmus. This endocrine gland produces thyroid hormones, namely triiodothyronine (T3) and thyroxine (T4), which influence various bodily functions
Thyroid Hormones and Their Role
Thyroid hormones act as messengers, affecting almost every cell and organ in the body. They control the rate at which cells convert oxygen and calories into energy, influencing metabolism, body temperature, heart rate, and more. Adequate thyroid hormone levels are essential for maintaining a healthy weight, proper growth and development, and overall well-being.
Analogous to a thermostat in a house, the pituitary gland acts as the control center for the thyroid gland. It produces thyroid-stimulating hormone (TSH), which signals the thyroid to release T3 and T4. This feedback loop ensures that the body’s thyroid hormone levels remain within a specific range.
Common Thyroid Disorders
Thyroid disorders encompass a range of conditions that affect the normal functioning of the thyroid gland. Two prevalent disorders are thyroid nodules, which are abnormal growths within the gland, and hyperthyroidism and hypothyroidism, which involve overactive and underactive thyroid function, respectively.
Thyroid Nodules: Causes and Symptoms
Hyperthyroidism: Causes, Symptoms, and Diagnosis
Hypothyroidism: Causes, Symptoms, and Diagnosis
Thyroid nodules are most commonly benign, but they can cause concern due to their potential to affect hormone production or become cancerous. Most nodules do not cause noticeable symptoms and are discovered incidentally during routine medical examinations. However, larger nodules may cause discomfort or visible swelling in the neck. It is essential to consult a healthcare provider for evaluation and appropriate management.
Hyperthyroidism occurs when the thyroid gland produces an excess of thyroid hormones. This overactivity can be caused by various factors, including an autoimmune disorder called Graves’ disease, thyroiditis, or the presence of thyroid nodules. Symptoms of hyperthyroidism may include unexplained weight loss, rapid heartbeat, irritability, and muscle weakness. Diagnosis involves a comprehensive medical history, physical examination, and thyroid function tests.
Hypothyroidism, on the other hand, refers to an underactive thyroid that does not produce sufficient thyroid hormones. Common causes include an autoimmune condition called Hashimoto’s thyroiditis, previous thyroid surgeries, or radiation therapy. Symptoms of hypothyroidism often include weight gain, fatigue, depression, and sensitivity to cold. Accurate diagnosis involves a thorough assessment of symptoms, physical examination, and thyroid function tests.
Diagnosing Thyroid Disorders
Accurate diagnosis is crucial for determining the appropriate treatment plan for thyroid disorders. Healthcare providers employ various diagnostic tools and methods to evaluate thyroid function and identify potential underlying causes.
Medical History and Physical Examination
During a medical consultation, your healthcare provider will conduct a comprehensive medical history assessment. This includes discussions about symptoms, past medical conditions, family history, and current medications. Additionally, a physical examination may be performed to assess the size and texture of the thyroid gland, as well as to check for other signs of thyroid dysfunction.
Thyroid Function Tests: An Essential Diagnostic Tool
Thyroid function tests are vital for evaluating thyroid hormone levels and detecting abnormalities. These tests typically measure the levels of TSH, T3, and T4 in the blood. Elevated or reduced hormone levels can indicate hyperthyroidism or hypothyroidism, respectively. Furthermore, additional blood tests may be conducted to assess thyroid antibodies, which can help identify autoimmune disorders affecting the thyroid gland.

Treatment Options for Thyroid Disease
The treatment approach for thyroid disease depends on the specific condition, severity of symptoms, and individual health factors. Medical professionals utilize various interventions to restore thyroid hormone balance, manage symptoms, and prevent potential complications.
Medication: Balancing Thyroid Hormone Levels
Radioactive Iodine Therapy: Targeting Hyperactive Thyroids
Surgical Procedures: Removing Thyroid Tissue or Tumors
For individuals with hypothyroidism, synthetic thyroid hormone replacement therapy is the standard treatment. This involves daily medication to provide the body with the necessary thyroid hormones. The dosage is adjusted based on regular monitoring of thyroid hormone levels and symptom improvement. In cases of hyperthyroidism, antithyroid medications may be prescribed to inhibit the excessive production of thyroid hormones. These medications help regulate hormone levels and manage symptoms. Close monitoring of thyroid function and potential side effects is crucial during this treatment.
Radioactive iodine therapy is commonly recommended for individuals with hyperthyroidism due to Graves’ disease or toxic nodules. This non-invasive procedure involves taking radioactive iodine orally, which is selectively absorbed by the overactive thyroid tissue. Over time, the radiation destroys the excess thyroid tissue, normalizing hormone production. Regular follow-up is necessary to monitor thyroid hormone levels and ensure treatment effectiveness.
In certain cases, surgical intervention may be required to treat thyroid disorders. Thyroid surgeries, such as thyroid lobectomy or total thyroidectomy, involve the partial or complete removal of the thyroid gland. These procedures may be necessary for treating thyroid cancers, large nodules causing compression, or when other treatment options are ineffective or contraindicated.
Lifestyle Changes and Management
In addition to medical interventions, lifestyle changes can significantly impact thyroid health and overall well-being. By adopting healthy habits, individuals can optimize their treatment outcomes and improve their quality of life.
Diet and Exercise: Supporting Thyroid Health
Maintaining a balanced diet rich in essential nutrients may be helpful for thyroid function. Including iodine-rich foods, such as seafood and seaweed, can support the production of thyroid hormones. Additionally, a diet abundant in fruits, vegetables, lean proteins, and whole grains provides the necessary nutrients for overall health. Regular exercise, tailored to individual capabilities, can also help regulate metabolism and support thyroid function.
Stress Management: Impact on Thyroid Function
Stress management plays a vital role in maintaining optimal thyroid function. Chronic stress can disrupt hormone balance and exacerbate symptoms of thyroid disorders. Engaging in relaxation techniques, such as meditation, yoga, or deep breathing exercises, can help reduce stress levels and promote overall well-being. Additionally, getting adequate sleep and practicing self-care activities can support the body’s ability to cope with stress.
Schedule a Consultation with us!
Thyroid disease is a complex condition that requires careful diagnosis and treatment. By understanding the role of the thyroid gland, recognizing common disorders, and exploring treatment options, individuals can actively participate in managing their thyroid health. Remember to schedule a consultation with one of our ENT doctors at Penn Medicine Becker ENT & Allergy for personalized advice and regular monitoring to ensure the effectiveness of treatment.

Pick one of our convenient locations
for your Thyroid Disease Treatment
