
Snoring & Sleep Treatment
If you or a loved one are struggling with snoring, Penn Medicine Becker ENT & Allergy has the expertise and resources to help. With the help of an experienced ENT doctor, you can begin to find relief from this disruptive sleep disorder. Whether it’s identifying the underlying causes of your snoring or finding the right treatment plan to address your specific needs, our team is here to provide comprehensive care and support.
Impact of Snoring
Snoring is the noise produced during sleep when the flow of air through the mouth and nose is partially blocked. It occurs when the tissues in the airway vibrate, resulting in the characteristic sound. Snoring can range from mild to severe, and it can be an occasional occurrence or a chronic problem.
In addition to diagnosing and treating snoring, Penn Medicine Becker ENT & Allergy offers lifestyle advice on how to reduce snoring. Weight loss, avoiding alcohol before bedtime, and sleeping on your side can all help reduce the severity of the condition. Our team can also provide tips on how to improve your sleep hygiene so that you get a better night’s rest. With our expertise and dedicated care, we can help you find relief from snoring and get the quality sleep you deserve.

Snoring Facts
- About 45% of people in the US snore at least sometimes, and 25% of people snore regularly.
- 90 million Americans suffer from snoring, and as many as half of those may have the sleep disorder Obstructive Sleep Apnea (OSA).
- Snoring is the third leading cause of divorce in the US behind infidelity and financial issues.
- The percentage of adults in the United States who snore varies by age group and region:
- By age group:
- 25-34: 19% snore, but do not have a partner who snores; 52% do not snore and do not have a partner who snores.
- 34-44: 18% snore, but do not have a partner who snores; 54% do not snore and do not have a partner who snores.
- 45-54: 23% snore, but do not have a partner who snores; 41% do not snore and do not have a partner who snores.
- 55-64: 29% snore, but do not have a partner who snores; 34% do not snore and do not have a partner who snores.
- By region:
- Northeast: 23% snore; 12% snore and have a partner who snores; 20% do not snore and do not have a partner who snores; 45% do not snore but have a partner who snores.
- South: 23% snore; 16% snore and have a partner who snores; 18% do not snore and do not have a partner who snores; 43% do not snore but have a partner who snores.
- By age group:
It’s worth noting that snoring can be light and occasional, or it can be a sign of a more serious health condition like obstructive sleep apnea (OSA). If you or a loved one is experiencing disruptive snoring or other sleep issues, it may be worth speaking with a doctor to determine the underlying cause and explore treatment options.
Causes of Snoring
Several factors can contribute to snoring. Here are some common causes:
Obstructive Sleep Apnea (OSA)
Nasal Passages and Nasal Congestion
Throat Muscles and Excess Tissue
Sleep Position
Alcohol Consumption and Sedatives
Excess Weight and Obesity
Nasal Polyps and Other Health Conditions
OSA is a sleep disorder characterized by pauses in breathing during sleep. It is caused by the partial or complete blockage of the upper airway, leading to snoring and interrupted sleep patterns.
Nasal congestion, caused by allergies, colds, or sinus infections, can obstruct the nasal passages, forcing individuals to breathe through their mouths and increasing the likelihood of snoring.
Weak throat muscles and excessive tissue in the throat can contribute to the narrowing of the airway, leading to snoring.
Sleeping in a supine position can lead to the backward collapse of the tongue and soft throat tissues, causing airway blockage and the common issue of snoring.
Alcohol intake and sedatives relax the throat muscles, which can lead to increased snoring.
Excessive weight and obesity can contribute to snoring due to the accumulation of fatty tissues around the throat, narrowing the airway.
Nasal polyps, as well as certain medical conditions such as chronic allergies or asthma, can cause nasal congestion and contribute to snoring.
Impact of Snoring on Health
Snoring can have various impacts on overall health, including:
Sleep Quality
Snoring often disrupts sleep, leading to restless sleep patterns and poor sleep quality.
Cardiovascular Disease
Chronic snoring, particularly when accompanied by pauses in breathing, can increase the risk of developing cardiovascular diseases such as hypertension (high blood pressure) and heart disease.
Morning Headaches and Sore Throat
Individuals who snore frequently may experience morning headaches and a sore throat upon waking due to the strain on their respiratory system.
Relationship Strain
Snoring can create tension and strain in relationships, as the loud snoring may disturb the sleep of the snorer’s bed partner.
Treatment Options for Snoring
Fortunately, there are various treatment options available to alleviate snoring and improve sleep quality. These include:
Lifestyle Changes
Making lifestyle changes such as losing excess weight, avoiding alcohol intake, and practicing good sleep hygiene can significantly reduce snoring.
Nasal Strips and Nasal Sprays
Nasal strips and sprays can help to open up the nasal passages, reducing congestion and improving the flow of air.
Oral Appliances
Mandibular advancement devices and mouth guards can be worn during sleep to reposition the jaw and tongue, helping to keep the airway open.
Positive Airway Pressure (PAP) Therapy
PAP therapy involves using a machine that delivers a continuous flow of air through a mask, keeping the airway open during sleep. This is commonly used for the treatment of obstructive sleep apnea.
Surgical Procedures
In some cases, surgical intervention may be necessary to remove excess tissue or correct structural abnormalities in the airway. Procedures like the pillar procedure can provide long-term relief for chronic snoring.
Radiofrequency ablation (RFA)
Is a minimally invasive procedure that uses radiofrequency energy to reduce the size of enlarged tissues in the throat and help reduce snoring.
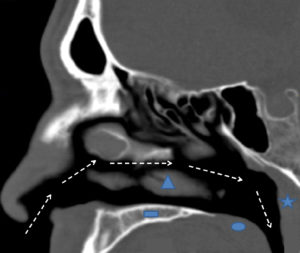
Anatomy of Snoring
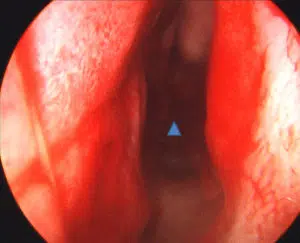
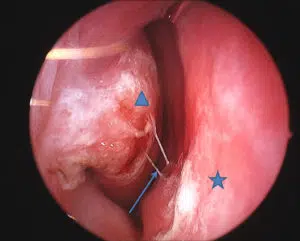
As noted above, snoring occurs when the soft tissues of the upper airway vibrate due to turbulent airflow. This turbulence may occur at the level of the nose, mouth, or throat (Figure 1). In the nasal airway, a deviated septum (Figures 2 and 3), enlarged inferior turbinates (Figure 4), or nasal valve collapse may all lead to irregular and choppy airflow. Further back in the nasal airway, enlarged adenoids may also block the air entering the nose. When air flows in through the mouth, it may experience obstruction due to an enlarged tongue, a long soft palate or uvula, or enlarged tonsils. In some cases, the tongue, palate, uvula and tonsils are all normal in size, but are crowded and collapse in the oral airway as a result of a smaller than usual jaw (or mandible). Further down in the neck, excess soft tissue in patients with a “thick” neck may lead to blockage and turbulence.


Schedule your consultation

Pick one of our convenient locations
for your Snoring & Sleep Treatment
