
Turbinate Surgery
When the inferior turbinates are enlarged, or hypertrophied, they can lead to bothersome nasal congestion, blockage, and obstruction. Evaluation of nasal blockage and congestion starts with a simple description of symptoms to your Ear, Nose, and Throat (ENT) doctor. At Penn Medicine Becker ENT & Allergy offers turbinate surgery at our multiple locations to patients with these symptoms.
Turbinate Anatomy and Function
There are 3 (sometimes 4) pairs of turbinates in the nose. These are the inferior, middle, superior, and – in some patients – supreme turbinates. The turbinates are made up of a bony skeleton surrounded by a mucosal lining, and they serve to heat and humidify the air that enters the nose. The lining of the inferior turbinates is particularly vascular and can become quite enlarged (or “hypertrophied”) at times. Swelling typically occurs as part of the normal nasal cycle which involves alternating enlargement (congestion and decongestion) of the turbinates on each side of the nose several times daily. However, in some patients, this swelling can be quite bothersome and may require treatment.

Further back in the nose, the middle turbinates mark the entryway to the sinus cavities. The middle turbinates are normally a straight, narrow, vertically-oriented structure, but they may become angled or enlarged in such a way that impacts the entry area to the sinuses. When curved towards the sinus areas, a middle turbinate is characterized as “Paradoxical.” When a middle turbinate is enlarged, this is usually due to inflation of the central component of the turbinate with air, and this is referred to as a “Concha Bullosa” or “air-filled bone”.
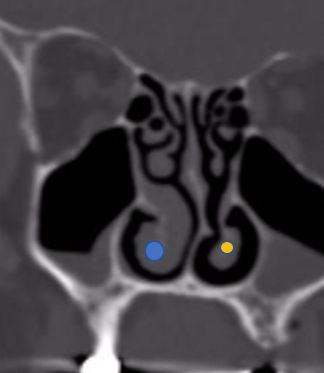
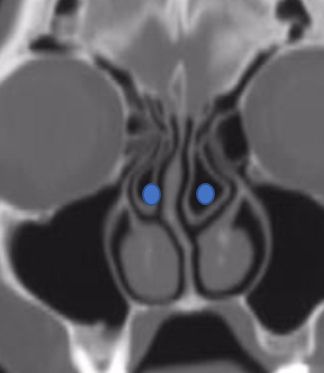
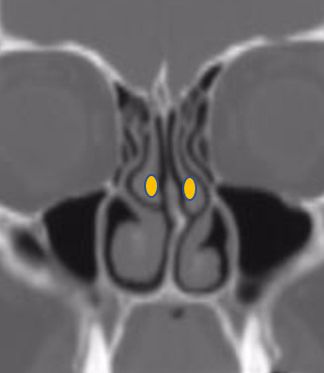
CT scans demonstrates concha bullosa (blue) compared to normal middle turbinates (yellow)
Evaluation and Medical Treatment for Enlarged Turbinates
When the inferior turbinates are enlarged, or hypertrophied, they can lead to bothersome nasal congestion, blockage and obstruction. Evaluation of nasal blockage and congestion starts with a simple description of symptoms to your Ear Nose and Throat doctor (ENT). The doctor will perform a thorough physical exam often including a nasal endoscopy to closely evaluate the nasal and sinus passages and to look for other potential sources of your nasal congestion. Sometimes the problem may be confined to the turbinates, but in other instances there may be other contributing factors such as a deviated septum, enlarged adenoids, or nasal and sinus polyps. Based on findings of the history and physical exam, further testing – such as allergy testing or a CT scan – may be ordered.
While some turbinate enlargement is part of the normal nasal cycle, other factors may make the turbinates unusually engorged. Allergies, inhaled environmental irritants (dust, smoke, etc.), or simple anatomical abnormality all may contribute to inferior turbinate hypertrophy. Medications designed to decrease turbinate hypertrophy are often used on a trial-and-error basis. Nasal corticosteroid sprays and nasal antihistamine sprays are often effective in decreasing inferior turbinate hypertrophy. Over-the-counter decongestant sprays (e.g., Afrin) are also effective but are only designed for short-term (1-3 days) use. Oral decongestants are less effective but may be tried for short-term use as well (assuming no other medical contraindications). In some patients, saline “Neti-pot”-like irrigation to decrease the presence of irritants in the nose may help.
Inferior Turbinate Surgery
When medications are ineffective and the inferior turbinates are hypertrophied and causing nasal blockage and congestion, surgical approaches may be an option. Surgery on the inferior turbinates focuses on diminishing the congested lining and moving or “out-fracturing” the turbinate bone to open up the nasal passage. While there are several techniques to minimize swelling of the turbinate mucosa, the two most commonly performed procedures are RadioFrequency Ablation (RFA) and Sub-Mucosal Reduction (SMR) of the inferior turbinates.
In the RFA procedure, a small probe is placed in the sub-mucosal area of the turbinate (between the inner turbinate bone and the outer mucosal lining) and low-power radiofrequency energy is applied to decrease tissue volume. The procedure is typically well tolerated and can be performed with a patient awake in the office setting. When performed on an awake patient, however, injection of the turbinate with numbing and vasoconstrictive agents (e.g., lidocaine with epinephrine) is standard. However, his injection of the inferior turbinates is documented to have some rare but significant visual complications due to the connection of the inferior turbinate blood supply with the blood supply of the eye.
In the SMR procedure, a small incision is made in the front part (or “head”) of the inferior turbinate. Dissection is performed, creating a pocket in the sub-mucosal lining for placement of a powered instrument known as a “micro-debrider.” The micro-debrider uses suction to pull in the engorged sub-mucosal tissue of the inferior turbinate so that it may be cut-down or “reduced” by its rotating blades. Once the sub-mucosal lining has been reduced, the healing process begins and scar tissue forms to prevent the lining from swelling as it had prior to surgery. Studies support SMR as effective in reducing nasal congestion while maintaining the warming and humidification function of the turbinates.
Either RFA or SMR may be accompanied by outfracture of the inferior turbinates. In outfracture, the inferior turbinate (“Conchal”) bone is firmly moved or “out-fractured” from its normal midline position to a more lateral position along the nasal sidewalls. In so doing, the central component of the nasal airway is opened up to allow for improved passage of air. Outfracture is typically performed under general anesthesia in conjunction with other turbinate and nasal procedures.
Middle Turbinate Surgery
When the middle turbinate is enlarged, it is known as a “Concha Bullosa.” A concha bullosa can be thought of as a balloon with turbinate bone on both sides surrounding an air-filled center. Typically the component of the bone closest to the midline (or septum) of the nose has the primary attachment to the skull base, and this part is preserved. The lateral wall – closest to the sinuses – is removed or resected using a combination of cutting and grasping forceps and powered instruments such as a micro-debrider. Resection of the lateral aspect of the concha bullosa typically opens up the central sinus drainage pathway and may relieve some obstruction of the sinus area.
Additional Procedures beside Turbinate Surgery
Inferior Turbinate surgery is typically performed to improve nasal airflow and reduce blockage and congestion. Sometimes, other components may contribute to these symptoms, and these components may be addressed at the same time as turbinate surgery. Deviated septum, sinus blockage, nasal and sinus polyps, enlarged adenoids, and nasal valve collapse are just some of the anatomical abnormalities that may also contribute to a patient’s nose and sinus symptoms. If these factors are part of a patient’s symptom profile, patients should discuss all concerns about turbinate reduction before and after surgery with the surgeon, and decide whether additional procedures are indicated and, if so, whether to perform them at the same time or at a later date.
Why Choose Our Specialists?
- Dr. Daniel G. Becker, Founder, and Medical Director of The Penn Medicine Becker ENT & Allergy Center, is a highly trained, board-certified specialist who graduated magna cum laude from Harvard College in 1986 and was awarded a full merit scholarship to attend the University of Virginia Medical School.
- Dr. Samuel S. Becker, Director of Rhinology at The Penn Medicine Becker ENT & Allergy Center, is a highly trained, board-certified specialist who graduated from Amherst College in 1991 and attended medical school at the University of California San Francisco.
- Dr. Kenneth Rosenstein is a highly trained, board-certified otolaryngologist who attended medical school at McGill University. Dr. Rosenstein specializes in ear, nose, and throat care, focusing on pediatric care, thyroid disease, hearing impairment, ear conditions, and voice and swallowing difficulties.
- Dr. Naomi Gregory is a highly trained, board certified otolaryngologist who specializes in the diagnosis and treatment of diseases of the ear, nose, and throat. Dr. Gregory completed medical school at the Philadelphia College of Osteopathic Medicine in Philadelphia PA.
- Dr. Michael Lupa, MD is a highly trained, board-certified otolaryngologist with additional training in sinus surgery and allergy treatment as well as advanced skull base surgery. He studied Biology at Tufts University and went on to complete medical school at Case Western University School of Medicine in Cleveland, Ohio.
- Dr. Robert Mignone is a highly trained, board-certified otolaryngologist-head and neck surgeon who attended medical school at New York College of Osteopathic Medicine.
- Dr. Aubrey McCullough is a highly trained otolaryngologist, facial plastic, and head and neck surgeon who completed medical school at Midwestern University Arizona College of Osteopathic Medicine.
- Dr. Luke Kim is an otolaryngologist who specializes in the diagnosis, medical management, and surgical treatment of diseases of the ear, nose, and throat. Dr. Kim graduated with honors and with distinction from Cornell University and completed his medical studies at the Perelman School of Medicine at the University of Pennsylvania.
- Dr. Omar Ahmed is a highly skilled otolaryngologist-head and neck surgeon who completed his medical training at Rutgers Robert Wood Johnson Medical School. He is known for his extensive expertise in sinus and nasal disorders and has contributed significantly to the field with over 20 published articles and book chapters.
- Dr. Gileno Fonseca is a highly trained otolaryngologist-head and neck surgeon who attended medical school at the University of Florida. Since 2022, it has been board-certified in Otolaryngology.
- Dr. Alisa Yamasaki is a highly trained Otolaryngologist–Head & Neck Surgeon who completed her undergraduate studies at Dartmouth College and her medical degree at Harvard Medical School. She also completed a fellowship in Facial Plastic and Reconstructive Surgery at the University of Michigan Medical Center.
Turbinate Surgery FAQs
This depends on the patient and surgeon preference as well as the type of procedure performed. SMR of the inferior turbinates, as well as outfracture, is typically performed with patients “asleep” under general anesthesia. RFA of the inferior turbinates may be performed with patients awake and anesthetized with injected medication (e.g., lidocaine).
When people think of packing, they often envision the historical use of nearly 20 feet of Vaseline-infused gauze that in the past was packed into the nose and removed after one week. This is rarely performed in today’s procedures. More commonly, a small, “postage-stamp” sized piece of absorbable hemostatic mesh (e.g., Surgicel) is placed to control bleeding at the end of surgery. This usually resorbs or washes away after a few days.
No. Turbinate surgery does not change the “outside” of the nose or face. After undergoing surgery, some people may experience minor swelling or bruising in their nose, but overall most people report positive results with turbinate reduction before and after surgery.
No. Surgery on the inferior turbinate does not involve stitches or sutures. On occasion, surgery on the middle turbinate (i.e., Concha bullosa) may involve stitches, although in most cases these are absorbable and do not require removal.
Most patients find that turbinate surgery alone is accompanied by mild discomfort which is typically managed with over-the-counter medication such as Extra Strength Tylenol. When accompanied by other nasal and sinus procedures, stronger pain medication may be needed for a short-term period.
The turbinates have a strong blood supply, and surgery may be accompanied by some post-operative bleeding. Before the procedure is completed, steps are taken by the surgeon to minimize post-operative bleeding. Most post-operative bleeding can be easily controlled with topical vasoconstrictor sprays such as Afrin or Oxymetazoline. However, you should always let your surgeon know immediately if you experience persistent or significant bleeding. Along these lines, it is also important to let your surgeon know of all medications and supplements you are taking before surgery, as well as any medical conditions you may have (e.g., bleeding or clotting disorders) as some of these may make bleeding more likely. Your surgeon may recommend discontinuing some of these medications for a period of time before and after surgery. If you have a bleeding or clotting disorder, your surgeon may recommend consultation with a hematologist prior to surgery.
Most patients take a few days off, depending on the specific procedure performed as well as the type of anesthesia involved. Procedures performed under local anesthesia (e.g., RFA) typically involve less recovery – maybe a day or 2 – before patients return to work. When patients have nasal and sinus procedures performed under general anesthesia, it is often advised that they prepare to take 3-4 days off of work. Specific details should be discussed with your surgeon.
While the procedures vary from patient to patient, turbinate surgery alone is quite brief and typically takes 15-20 minutes for the actual procedure. Times, of course, lengthen when other, complementary procedures (e.g., septoplasty, sinus surgery, etc.) are performed.
If you live in the states of New Jersey or Pennsylvania, Penn Medicine Becker ENT & Allergy Center offers turbinate surgery among its services. For a full list of services, please visit our Locations page.

