
Septoplasty
Septoplasty is a surgical procedure that targets the correction of a deviated nasal septum, which occurs when the cartilage and bone wall that separates the two sides of the nose is misaligned. This condition can lead to nasal obstruction, difficulty breathing, frequent sinus infections, nasal congestion, impaired sense of smell, and facial pain. In severe cases, it may also be linked to sleep apnea. The main goal of septoplasty surgery is to straighten the septum, ultimately improving the patient’s quality of life.
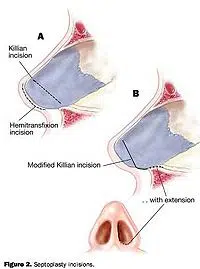
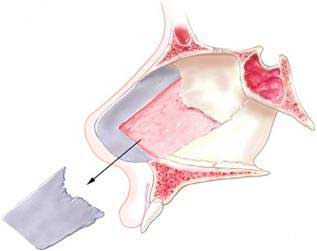
The procedure begins when the surgeon makes an incision inside the nose to gain access to the nasal tissue and bones that make up the septum. The surgeon will then carefully remove any excess tissue or crooked cartilage that is obstructing the nasal cavity. If necessary, the doctor may need to replace broken pieces of bone with new pieces before properly realigning them. Once the surgeon completes all adjustments and has correctly repositioned the septum in its original position, it will be secured by sutures or stitches and/or special surgical glue to help hold it in place.

After the surgery, your doctor may suggest inserting some type of nasal packing into your nostrils to prevent excessive bleeding during recovery time. Depending on your specific condition, you may need antibiotics and pain medications following surgery as well as an additional follow-up visit with your physician for further evaluation.
Most people typically recover from septoplasty with no major issues or complications, such as breathing difficulties or increased infection risk. However, this type of procedure carries potential risks including infection and scarring, which could lead to more serious problems down the road if not managed properly by a medical professional.
Benefits of Septoplasty
Septoplasty is a surgical procedure that targets the correction of a deviated nasal septum, when the cartilage and bone wall separating the two sides of the nose are misaligned. This condition can lead to nasal obstruction, difficulty breathing, frequent sinus infections, nasal congestion, impaired sense of smell, and facial pain. The main goal of septoplasty surgery is to straighten the septum to improve airway flow as well as reduce congestion.
The benefits of septoplasty are numerous for those with a deviated nasal septum who are looking for symptom relief. By realigning the nasal passages, patients can experience better overall breathing and an improved sense of smell. Additionally, this outpatient procedure can also fix a broken nose or other aesthetic issues associated with the problem to provide both medical and cosmetic benefits at once!
Furthermore, septoplasty is ideal for those who want relief from nasal obstruction-related issues such as chronic runny nose or frequent bouts of sinusitis due to blocked nasal passages that can lead to increased risk for infection. If you fit these criteria, then you may be an ideal candidate for this type of surgery!
When considering a septoplasty procedure, you should seek out a reputable plastic surgeon who can answer all your questions about potential risks and outcomes before making any decisions. It’s also important for the surgeon to perform these types of surgeries in an accredited surgery center that typically boasts state-of-the-art technology and safety procedures when performing these procedures.
Conditions Treated With Septoplasty
Septoplasty is a plastic surgery procedure that treats a crooked septum, which can cause difficulty in nasal breathing. During this medical procedure, the surgeon will make an incision inside the nose and remove any excess tissue or crooked cartilage that is obstructing the nasal cavity. The surgeon will then carefully align and secure the septum in its original position with sutures or specialty surgical glue. This procedure can help improve airway flow, reduce congestion, and provide relief from associated symptoms such as chronic runny nose and frequent sinus infections due to blocked nasal passages.
Diagnosis Process for Determining Candidacy for Surgery
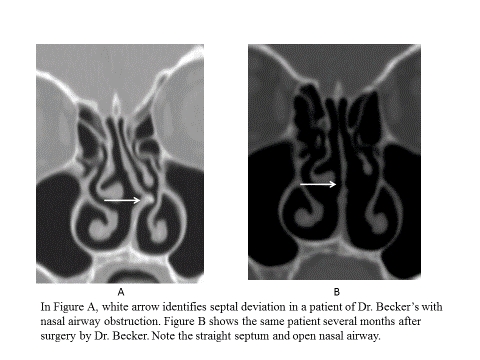
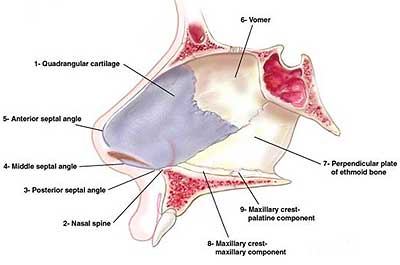
To determine candidacy for septoplasty surgery, a plastic surgeon will first need to review the patient’s medical history and assess their symptoms via a physical exam. This often includes nasal airway inspection in which the doctor uses a nasal endoscope while measuring the patient’s nasal septum. The provider may also use imaging (such as X-rays or CT scans) to get a better visual of the nose anatomy and further evaluate the deviated septum. Additionally, if allergies are suspected, the doctor may recommend allergy testing to rule out any allergic reactions that could worsen nasal obstruction if left untreated. Lastly, a clinical trial may also be performed to make sure that other medical treatments have been exhausted prior to considering surgery as an option.
A reputable plastic surgeon will best serve patients who may be candidates for septoplasty surgery. With experience and state-of-the-art processes, an experienced doctor will be able to accurately diagnose patients who need this type of nasal surgery and can provide patients with a clear treatment plan.
The Procedure Itself
Septoplasty is a relatively straightforward procedure that typically takes 1 to 2 hours when performed by an experienced plastic surgeon. The surgeon will first make a small incision inside the nostrils to access the septum. The provider may use specialized tools to remove any crooked or excess cartilage from the septum. In some cases, the surgeon may also need to reposition the bone and cartilage before securing it with sutures or surgical glue. After achieving proper alignment, the surgeon will close up the incision and provide post-operative instructions for recovery.
For the procedure, patients may receive either local or general anesthesia depending on their preference and medical history. Additionally, post-operative care is essential for promoting overall healing and ensuring successful results from surgery. This often includes restful sleep, cold compresses for swelling relief, avoiding activities that could result in nasal trauma until complete healing has occurred, and using a humidifier while sleeping to keep nose passages hydrated.
Aftercare Instructions Following Surgery
Following a septoplasty procedure, patients must take proper aftercare measures to ensure successful results. They should get plenty of rest and avoid activities that could cause injury or trauma to the nose. Patients may use over-the-counter pain medications as needed to alleviate discomfort. Additionally, cold compresses can help reduce swelling, and patients should use a humidifier while sleeping for hydration purposes. Patients should also avoid blowing their nose during recovery and closely follow all post-operative instructions provided by their plastic surgeon to get optimal results from the surgery.
Risks of Septoplasty
Although Septoplasty is a relatively safe procedure, it still has some associated risks. The most common risks include infection, bleeding, and scarring at the incision site inside the nose. In some cases, patients may also experience numbness in the nasal area due to nerve damage, which can be temporary or permanent depending on the individual. Additionally, there is also a risk of septal hematoma (a collection of blood) forming after surgery, which could cause further obstruction if not treated promptly. Other rare but possible risks associated with septoplasty include septal perforation (a hole in the septum), exposure of cartilage grafts, and damage to surrounding structures such as facial sinuses or tear ducts.
Patients should discuss any potential risks or complications with their plastic surgeon prior to undergoing septoplasty so that they can make an informed decision about their treatment plan. Individuals should follow all of their surgeon’s pre- and post-operative instructions to minimize potential side effects from surgery.
Why Choose Our Specialists?
- Dr. Daniel G. Becker, Founder, and Medical Director of The Penn Medicine Becker ENT & Allergy Center, is a highly trained, board-certified specialist who graduated magna cum laude from Harvard College in 1986 and was awarded a full merit scholarship to attend the University of Virginia Medical School.
- Dr. Samuel S. Becker, Director of Rhinology at The Penn Medicine Becker ENT & Allergy Center, is a highly trained, board-certified specialist who graduated from Amherst College in 1991 and attended medical school at the University of California San Francisco.
- Dr. Kenneth Rosenstein is a highly trained, board-certified otolaryngologist who attended medical school at McGill University. Dr. Rosenstein specializes in ear, nose, and throat care, focusing on pediatric care, thyroid disease, hearing impairment, ear conditions, and voice and swallowing difficulties.
- Dr. Naomi Gregory is a highly trained, board certified otolaryngologist who specializes in the diagnosis and treatment of diseases of the ear, nose, and throat. Dr. Gregory completed medical school at the Philadelphia College of Osteopathic Medicine in Philadelphia PA.
- Dr. Michael Lupa, MD is a highly trained, board-certified otolaryngologist with additional training in sinus surgery and allergy treatment as well as advanced skull base surgery. He studied Biology at Tufts University and went on to complete medical school at Case Western University School of Medicine in Cleveland, Ohio.
- Dr. Robert Mignone is a highly trained, board-certified otolaryngologist-head and neck surgeon who attended medical school at New York College of Osteopathic Medicine.
- Dr. Aubrey McCullough is a highly trained otolaryngologist, facial plastic, and head and neck surgeon who completed medical school at Midwestern University Arizona College of Osteopathic Medicine.
- Dr. Luke Kim is an otolaryngologist who specializes in the diagnosis, medical management, and surgical treatment of diseases of the ear, nose, and throat. Dr. Kim graduated with honors and with distinction from Cornell University and completed his medical studies at the Perelman School of Medicine at the University of Pennsylvania.
- Dr. Omar Ahmed is a highly skilled otolaryngologist-head and neck surgeon who completed his medical training at Rutgers Robert Wood Johnson Medical School. He is known for his extensive expertise in sinus and nasal disorders and has contributed significantly to the field with over 20 published articles and book chapters.
- Dr. Gileno Fonseca is a highly trained otolaryngologist-head and neck surgeon who attended medical school at the University of Florida. Since 2022, it has been board-certified in Otolaryngology.
- Dr. Alisa Yamasaki is a highly trained Otolaryngologist–Head & Neck Surgeon who completed her undergraduate studies at Dartmouth College and her medical degree at Harvard Medical School. She also completed a fellowship in Facial Plastic and Reconstructive Surgery at the University of Michigan Medical Center.
- Breathe Easy: How to Fix a Deviated Septum Once and for All
- Septoplasty Recovery Day-by-Day Timeline
- Snoring – 5 Treatment Possibilities

