Angiotensin-converting enzyme (ACE) inhibitors are a class of medications widely used to treat various health conditions.
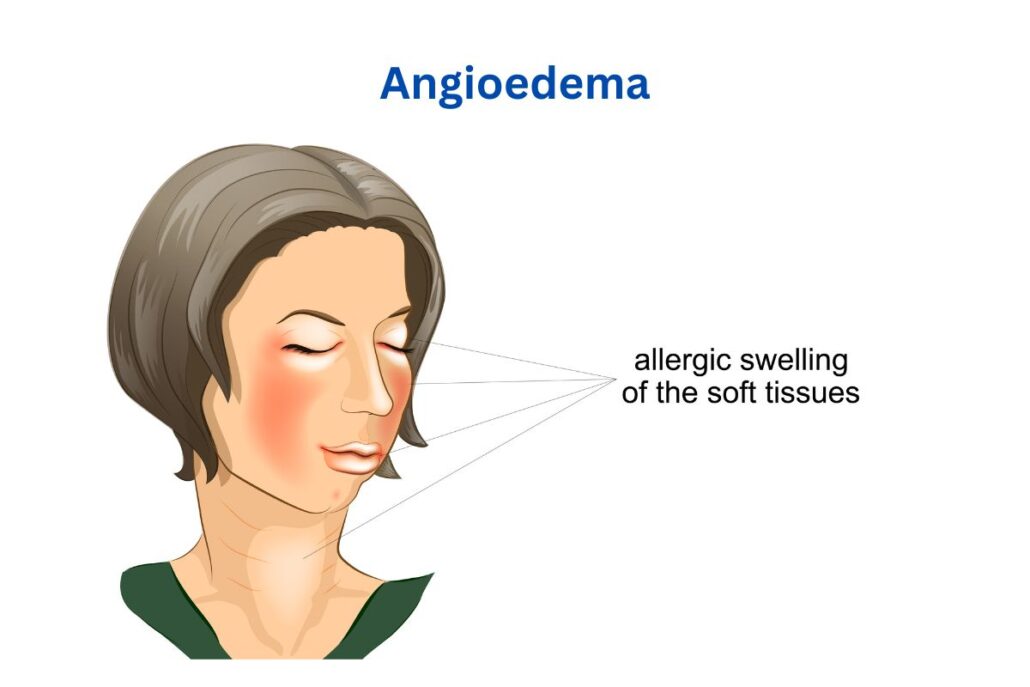
However, they can cause angioedema, a serious side effect characterized by the localized swelling of the deep dermis, subcutaneous, or submucosal tissue. Around 0.1%–0.7% of patients who are undergoing ACE inhibitor therapy are estimated to experience Angioedema. ACEI is a common cause worldwide for patients arriving at the emergency department with angioedema.
This post aims to provide an in-depth understanding of why ACE inhibitors cause angioedema while covering the mechanisms involved in angiotensin-converting enzyme inhibitor-induced angioedema.

What Angioedema From ACE Inhibitors Might Look Like
| Symptom | What It Feels or Looks Like |
|---|---|
| Swelling of lips, tongue, or throat | Sudden puffiness, feels tight or full, may affect talking or eating |
| Difficulty breathing | Shortness of breath, wheezing, or tight chest |
| Hoarseness or voice changes | Voice sounds different, strained, or quieter |
| Skin swelling without a rash | Puffy face or hands with no itching or redness |
| Stomach pain (rare) | Sudden cramps, bloating, or discomfort without a clear reason |
What ACE Inhibitors Do and Why They’re Prescribed
Angiotensin-converting enzyme inhibitors are a category of medications that have a significant role in the medical field, particularly in treating high blood pressure, also known as hypertension and heart failure.
They function by inhibiting the activity of the angiotensin-converting enzyme, a critical enzyme in the renin-angiotensin system. This system regulates blood pressure and fluid balance within the body, making it a key target for antihypertensive medications.
Common Conditions Treated With ACE Inhibitors
ACE inhibitors are mainly used to treat high blood pressure and heart-related problems.
If you’ve been prescribed an ACE inhibitor, it’s likely to help manage one of the following:
- High blood pressure (hypertension) – These medications help relax your blood vessels so your heart doesn’t have to work as hard.
- Heart failure – ACE inhibitors make it easier for your heart to pump blood by reducing stress on the heart.
- Coronary artery disease or after a heart attack – They help prevent further damage to your heart and improve long-term outcomes.
- Kidney problems from diabetes (diabetic nephropathy) – These drugs can help protect your kidneys, especially if you have diabetes.
Doctors often choose ACE inhibitors because they’re reliable, widely used, and shown to reduce the risk of serious problems like heart attacks and kidney failure. If you’re unsure why you’re taking them, it’s always okay to ask your doctor for a quick explanation.
Why Do ACE Inhibitors Cause Angioedema?
ACE inhibitors can, unfortunately, lead to a serious side effect known as angioedema. This condition is characterized by rapid skin swelling, mucous membranes, and submandibular tissues.
It’s a form of bradykinin-mediated angioedema that can occur without the presence of urticaria, a type of skin rash. The development of angioedema from ACE inhibitors results from the medication’s impact on a peptide called bradykinin.
ACE inhibitors block the degradation of bradykinin, leading to its accumulation in the body. This build-up of bradykinin in tissues, a phenomenon also known as ACE-I-induced angioedema triggers vasodilation, or the widening of blood vessels. This process, in turn, leads to fluid extravasation into deep tissues, which causes swelling.
Mechanism of Action of ACE inhibitors
The mechanism of action of ACE inhibitors involves the role of the angiotensin-converting enzyme in the production of angiotensin II and the degradation of bradykinin.
Vasodilation and Blood Pressure Regulation
Angiotensin-converting enzyme inhibitors, or ACE inhibitors as they are more commonly known, function by blocking the conversion of angiotensin I to angiotensin II.
Angiotensin II is a potent vasoconstrictor, meaning it can narrow the blood vessels, thereby increasing blood pressure.
This is a critical process in the body’s regulation of blood pressure, as well as the regulation of fluid balance.
Accumulation of Bradykinin
ACE inhibitors can cause angioedema because they increase bradykinin, a chemical that triggers swelling.
Normally, your body breaks down bradykinin with an enzyme that ACE inhibitors block. When bradykinin builds up, it makes your blood vessels more leaky, causing fluid to move into deeper tissues—like your lips, tongue, or throat.
This type of angioedema is different from allergic reactions. It usually happens without itching or hives and is directly linked to the way ACE inhibitors affect your system.
Bradykinin and Angioedema
The accumulation of bradykinin in the body can lead to angioedema. This condition is characterized by localized swelling of the deep dermis, subcutaneous, or submucosal tissue caused by the vascular extravasation of fluid into the interstitium.
The body’s most commonly affected areas include the face, tongue, lips, throat, and in severe cases, the airways, leading to potential airway compromise.
What Increases the Risk of Angioedema With ACE Inhibitors
While any individual taking ACE inhibitors can develop angioedema, certain factors increase the risk.
Studies have shown that individuals of African descent, particularly African Americans, are at a higher risk for developing ACE inhibitor-induced angioedema. This risk is also elevated in women, smokers, and people over the age of 65.
In addition to these demographic factors, certain medical conditions and histories can also increase the likelihood of experiencing episodes of angioedema. Similarly, a history of drug rash or adverse drug reactions can heighten the risk.
For instance, a history of angioedema, whether it be hereditary angioedema, idiopathic angioedema, or drug-induced angioedema, can predispose an individual to ACE inhibitor-associated angioedema.
Seasonal allergies, which can trigger hypersensitivity reactions, can also contribute to the risk. Interestingly, the incidence of angioedema among patients with diabetes mellitus is significantly decreased, suggesting a protective effect against ACE inhibitor-induced angioedema in this population.
Find Answers and Relief From ACE Inhibitor-Related Angioedema
Our Team Specializes in Identifying the Root Causes and Offering Safer, Effective Treatment Options.
When To Call an ENT and Allergy Specialist About ACE Inhibitor Reactions

Angioedema, specifically ACE inhibitor-induced angioedema, is a serious side effect that can lead to adverse reactions and requires immediate medical attention. Characteristics of Angioedema associated with ACE inhibitors are rapid skin swelling, abdominal pain, mucosa, and submucosal tissues. The swelling can occur in various body parts, but it is particularly concerning when it affects the throat or tongue.
This is because the swelling from ACE inhibitor-related angioedema among users can lead to airway swelling, making breathing difficult and potentially causing a life-threatening situation. In severe episodes of angioedema, the swelling can progress to the upper airway, leading to upper airway obstruction.
Upper airway obstruction is a critical situation that requires immediate intervention, often in the form of emergency airway management. In such cases, the patient may need a breathing tube to maintain an open airway. In severe cases, patients may need to be admitted to the emergency department of the closest hospital and may need to discontinue ACE inhibitors.
Options If ACE Inhibitors Are Causing Trouble
If ACE inhibitors are causing angioedema, your doctor may switch you to a different medication called an ARB.
ARBs (angiotensin receptor blockers) treat the same conditions—like high blood pressure and heart failure—but work differently and don’t raise bradykinin levels, which means they’re much less likely to cause swelling.
If you’ve had swelling while on an ACE inhibitor, tell your doctor right away. They might also recommend antihistamines to manage the reaction, especially if it’s mild.
For serious swelling—like trouble breathing or a swollen tongue—call 911 or go to the ER immediately.
If the swelling of your ACE inhibitor-induced angioedema is serious, contact emergency services immediately. If you’re looking for a clinic in Mt. Laurel, NJ, to help with mild episodes before they become more serious, please contact us today and schedule a consultation. Our Mt. Laurel clinic also serves the areas of Moorestown, Willingboro, Medford, and Palmyra.

