
Swallowing Disorders Treatment
Swallowing disorders can be a serious and life-altering condition, but with the right treatment from Penn Medicine Becker ENT & Allergy’s expert team of ENT doctors, it can be managed. Swallowing disorders can be caused by a variety of factors, such as nervous system disorders or other medical conditions. Diagnostic tests, including barium swallow and endoscopy, are used to determine the exact cause of the disorder. Treatment options depend on the cause and severity of the disorder and may include specialized swallowing exercises, speech therapy, medication, and/or surgery.
What Are the Symptoms of a Swallowing Disorder?
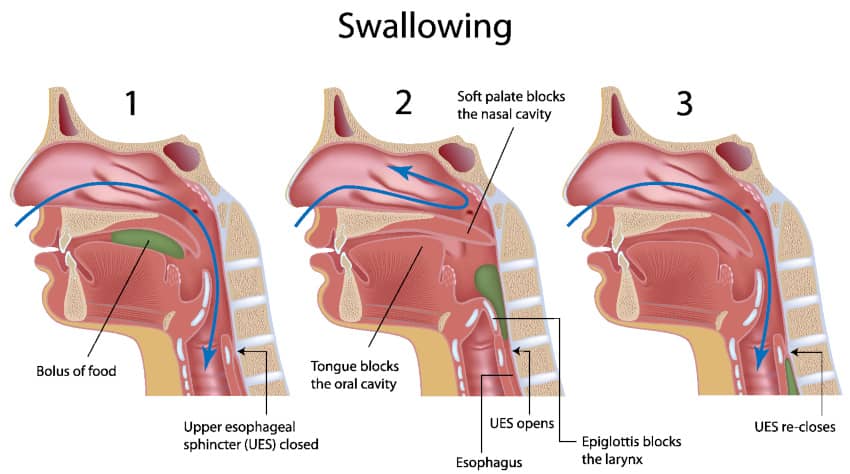
Swallowing disorders refer to conditions that affect a person’s ability to swallow safely and efficiently. These disorders can occur at any stage of the swallowing process, which involves the movement of food and liquid from the mouth to the stomach. Swallowing disorders can be categorized into two main types: oropharyngeal dysphagia and esophageal dysphagia.
Oropharyngeal dysphagia occurs when there are difficulties in the oral cavity or pharynx, which is the area at the back of the throat. This type of swallowing disorder is often associated with neurological disorders, muscular dystrophies, or structural abnormalities.
Esophageal dysphagia, on the other hand, is characterized by difficulties in the esophagus, the muscular tube that carries food from the throat to the stomach. This type of swallowing disorder can be caused by conditions such as gastroesophageal reflux disease (GERD), esophageal cancer, scar tissue, or esophageal sphincter dysfunction. Evaluation of esophageal dysphagia involves assessing the various factors that contribute to swallowing difficulties during the esophageal phase. This may include diagnostic procedures like esophageal manometry or endoscopy to evaluate the function and structure of the esophagus.

Causes of Swallowing Disorders
Swallowing disorders can have various underlying causes. Some common factors that contribute to these disorders include:
Neurological Disorders
Conditions like cerebral palsy, Parkinson’s disease, or stroke can affect the nerves and muscles involved in swallowing, leading to difficulties.
Structural Abnormalities
Certain structural abnormalities in the oral cavity, throat, or esophagus can impede the normal swallowing process.
Medical History
Individuals with a history of radiation therapy, cancer treatments, or surgery in the head, neck, or chest region may experience swallowing difficulties.
Muscular Dystrophies
Progressive muscle weakness in conditions like muscular dystrophy can affect the muscles responsible for swallowing.
Esophageal Disorders
Conditions such as GERD, esophagitis, or esophageal strictures can cause narrowing or inflammation of the esophagus, leading to swallowing problems.
Neurological damage
The abrupt onset of neurological impairment, such as a stroke or injury to the brain or spinal cord injury, has the potential to disrupt the coordination of swallowing, resulting in a condition known as oropharyngeal dysphagia.
Cancer and tumors
Depending on their specific location, certain forms of cancer, such as those affecting the neck or involving tumors, have the potential to cause oropharyngeal dysphagia.
Radiation
Following the administration of radiation therapy for specific cancer types like pharyngeal cancer, tonsillar cancer, and base of tongue cancer, individuals may experience the development of oropharyngeal dysphagia. This condition arises from the stiffening of the swallowing muscles resulting from radiation-induced effects.
Age
With advancing age, it is common to encounter a gradual weakening of the muscles in the throat. This weakening can potentially result in challenges related to the timely coordination of swallowing for certain individuals.
Muscle Tension Dysphagia
For some people, tension in the throat with the extrinsic laryngeal muscles can lead to difficulty swallowing or a constant lump in the throat sensation. This is due to the tension and recruitment constantly being placed on the muscles meant for swallowing, which can make it difficult for the swallowing mechanism to function normally. Evaluation of dysphagia, including neck cancer, involves assessing the wide variety of symptoms and their impact on swallowing function. The goals of dysphagia therapy aim to address these challenges and restore optimal swallowing function.
Symptoms of Swallowing Disorders
The symptoms of swallowing disorders can vary depending on the underlying cause and the stage of the swallowing process affected. Some common symptoms include:
- Difficulty Swallowing: The sensation of solid food getting stuck in the throat or chest.
- Painful Swallowing: Discomfort or pain while swallowing, also known as odynophagia.
- Weight Loss: Unexplained weight loss due to inadequate nutrition.
- Regurgitation: Food or liquid coming back up into the mouth after swallowing.
- Coughing or Choking: Coughing or choking during or after eating or drinking.
- Aspiration Pneumonia: Recurrent pneumonia caused by the inhalation of food or liquid into the lungs.
- Gastrointestinal Issues: Symptoms like acid reflux, heartburn, or vomiting.
- Dry Mouth: Decreased saliva production, leading to dry mouth and difficulty in swallowing dry foods.
- Respiratory Problems: Shortness of breath or wheezing after eating or drinking.
If you or a loved one experience any of these symptoms, it is essential to consult a healthcare provider for a proper diagnosis and treatment.
Diagnosis of Swallowing Disorders
Diagnosing swallowing disorders typically involves a multidisciplinary approach, with the involvement of healthcare professionals such as speech-language pathologists, gastroenterologists, and radiologists. The diagnostic process may include:
Medical History
Physical Examination
Swallowing Evaluation
Imaging Tests
Endoscopic Procedures
The healthcare provider will review the patient’s medical history, including any past surgeries, radiation therapy, or underlying conditions.
A thorough examination of the oral cavity, throat, and neck may be conducted to assess any structural abnormalities.
A speech-language pathologist may perform a swallowing evaluation, which can include observing the patient while eating or drinking, assessing the strength and coordination of swallowing muscles, and conducting special tests such as a barium swallow using a flexible tube. The flexible tube allows for a detailed examination of the swallowing process and helps in identifying any abnormalities or difficulties.
Radiological tests like a barium swallow or a modified barium swallow study can provide detailed images of the swallowing process and help identify any abnormalities.
In some cases, an endoscopy may be performed to visualize the esophagus and assess for any strictures, tumors, or inflammation. In the initial consultation you’ll have an endoscopic evaluation to know if you are an ideal candidate. In some cases, we may recommend that you meet with our Speech Language Pathology colleagues so that they may perform a Functional Endoscopic Evaluation of Swallowing (FEES).
Treatment Options for Swallowing Disorders
The treatment of swallowing disorders depends on the underlying cause and the specific swallowing difficulties experienced by the individual. It often involves a combination of therapeutic approaches and lifestyle modifications. Some common treatment options include:
Diet Modification
Altering the texture or consistency of food and liquids to make swallowing easier and safer. This may involve consuming pureed or mashed foods, thickened liquids, or using a feeding tube in severe cases.
Swallowing Exercises
Working with a speech-language pathologist to improve swallowing function and coordination through specific exercises and techniques.
Medications
Depending on the cause of the swallowing disorder, medications such as proton pump inhibitors or prokinetic agents may be prescribed to manage symptoms like acid reflux or esophageal spasms.
Surgical Interventions
In certain cases, surgical procedures may be required to correct structural abnormalities or remove obstructions in the esophagus.
Lifestyle Changes
Making lifestyle adjustments like maintaining good oral hygiene, avoiding triggers that worsen symptoms (e.g., spicy foods, caffeine), and quitting smoking can help manage swallowing difficulties.
Postural Techniques
Adopting specific positions while eating or drinking to facilitate swallowing and prevent aspiration.
It is crucial for individuals with swallowing disorders to work closely with a healthcare provider and a multidisciplinary team to develop a comprehensive treatment plan tailored to their specific needs.
Schedule your consultation

Pick one of our convenient locations
for your Swallowing Disorders Treatment
