
Nasal Polyps Treatment
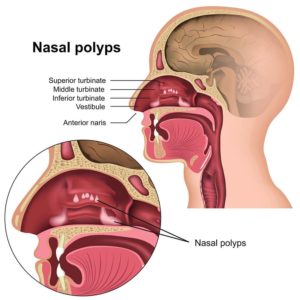
Nasal polyps are inflammatory growths in the nose and sinuses that can obstruct the nose and sinuses, leading to nasal blockage, recurrent infections, and loss of sense of smell and taste. Nasal polyps can also cause other sinus symptoms including headaches, snoring, nasal congestion, and sinus drainage. They’re may be related to asthma, recurrent infections, allergies, drug sensitivity, or underlying immune disorders. Nasal polyps are most commonly found in adults. They may be treated successfully with medications, but if not, then surgical removal may be required. Polyps frequently recur even after successful treatment. For this and other reasons, a specialist must evaluate nose and sinus symptoms.
Physicians at the Penn Medicine Becker ENT & Allergy Center can perform a complete fiberoptic evaluation of your nose to determine if any polyps are visible. If polyps are present, the physicians will discuss a wide range of treatment options with you. Often, taking simple medications can result in significant improvement and symptom resolution. Recent technology has made these treatments generally more effective, safer, and more comfortable than ever before. For more information on surgery for nasal polyps, see Dr. Becker’s published paper, The Surgical Management of Nasal Polyps.
When to See a Doctor
If you’re experiencing this condition, you should definitely see a doctor, especially if your nasal polyps symptoms last more than 10 days. Nasal polyps can be associated with other conditions such as allergies, sinus infections, asthma, to name a few.
Understanding the Underlying Causes of Nasal Polyps
Genetic Predisposition and Environmental Interactions
Emerging research suggests a significant genetic component to nasal polyps, with certain genes making individuals more susceptible to chronic sinusitis and polyp formation. A study published in the “Journal of Allergy and Clinical Immunology” identified specific genetic markers associated with an increased risk of developing chronic rhinosinusitis with nasal polyps. This research opens the door to personalized medicine approaches, where treatments can be tailored based on an individual’s genetic makeup.
Environmental factors may play a crucial role in the development of nasal polyps as well. Exposure to pollutants, cigarette smoke, and occupational hazards can exacerbate inflammation in the nasal passages and sinuses, and may contribute to polyp growth. A comprehensive review in “Environmental Health Perspectives” highlights the interaction between genetic predisposition and environmental triggers, suggesting that reducing exposure to harmful substances could mitigate the risk of polyps in genetically susceptible individuals.
The Role of the Microbiome in Nasal Health
The nasal microbiome, the community of microorganisms residing in the nasal cavity, has recently come under scrutiny for its potential role in nasal polyp formation. An imbalance in these microbial communities can lead to increased inflammation and polyp development. Research in “The Lancet Microbe” has demonstrated that individuals with nasal polyps often have a significantly altered nasal microbiome compared to those without polyps. These findings suggest that restoring a healthy microbial balance could be a novel approach to preventing or treating nasal polyps.
Immunological Insights: Beyond Allergies
While allergies may contribute to nasal polyp development, recent studies have broadened our understanding of the immunological aspects of polyps. Chronic inflammation, driven by a complex interplay of immune cells and signaling molecules, is at the heart of polyp formation. Innovative research published in “Nature Immunology” has identified specific immune pathways that are overactive in patients with nasal polyps. Targeting these pathways with new therapeutic agents could offer more effective treatments for patients who do not respond to traditional therapies.
Recognizing Nasal Polyps: Symptoms Indicating Advanced Treatment Needs
Some common symptoms of polyps include:
- Decrease in smell and/or taste
- Nasal blockage and congestion
- Runny nose
- Sneezing
- Postnasal drip
- Sinus pressure
- Fatigue
If you notice any of these symptoms, it is advisable to seek medical attention from your healthcare provider. The sooner you seek treatment, the sooner a diagnosis may be made and treatment can begin.

Schedule your consultation
Nasal Polyps Diagnosis and Tests
Nasal polyps usually appear during diagnostic rhinoscopy exams. They’re often associated with trouble breathing through the patient’s nostrils and may cause patients to lose or have a diminished sense of taste and/or smell.
Your doctor at Becker ENT and Allergy may evaluate these and other signs and perform an exam of your nose. If necessary, he or she may use a special lighted nasal device (endoscope) to examine your nose for polyps.
You may be advised by your physician to undergo additional tests, which include a nasal endoscopy to examine your nose and mouth, a CT scan to measure its size, shape, and position, or allergy tests to help identify other contributing factors to your symptoms.
Advanced Treatment Options for Nasal Polyps
There are no known cures for nasal polyps. However, some treatments are used to relieve symptoms. These include medications, surgery, and endoscopic procedures. Medications can help reduce swelling and inflammation. Surgery may be recommended for some cases but is intended as a means to open up the nasal and sinus cavities to allow topical medications to work effectively. Surgery is not a cure for nasal polyps.
Propel

Millions of people suffer from nasal polyps or chronic sinusitis. There are many different treatment options available, but not everyone responds well to them. One option for addressing these two conditions is the Propel sinus implant after a sinus procedure or SINUVA sinus implants.
The Propel stent is commonly placed during FESS, or functional endoscopic sinus surgery, to decrease the swelling and assist in the healing of the sinus passages. When you have chronic sinusitis, normal drainage is often prevented due to sinus passage inflammation. During surgery, these passages are enlarged. However, in some cases, post-surgical scarring can occur, and polyps may regrow, leading to a return of sinus inflammation, swelling, and, in some cases, infections.
This is where a Propel implant can make a difference. After completing the surgery, the Propel sinus implant is inserted. It is a spring-like device that helps to keep your sinuses open. The implant also contains mometasone furoate, a type of medication, which releases slowly to limit polyp regrowth and scarring to promote healing. Over the course of about one month, the implant will dissolve.
This is where a Propel implant can make a difference. After completing the surgery, the Propel sinus implant is inserted. It is a spring-like device that helps to keep your sinuses open. The implant also contains mometasone furoate, a type of medication, which releases slowly to limit polyp regrowth and scarring to promote healing. Over the course of about one month, the implant will dissolve.
During FESS surgery, you are typically given general anesthesia so that you are asleep and can feel no discomfort. Once you are anesthetized, an endoscope is inserted into your nostrils to allow the surgical team to visualize the area. Precision surgical instruments are then used to reposition or remove any necessary tissue. Once the procedure is completed, the implant is placed to keep the sinuses open.
In most cases, FESS is performed as an outpatient procedure, so you can go home the same day. For about a week, you may experience minor pain, swelling, and stuffiness. Your surgeon will provide detailed recovery instructions and any necessary medications to promote healing and recovery.
Sinuva
Sinuva is an implant designed for patients who are over the age of 18, have nasal polyps, and have a history of ethmoid sinus surgery. This technology may be an option if you do not want to repeat sinus surgery.
Once the implant is in place, it begins to release mometasone furoate, a medicine that works to alleviate inflammation and nasal polyps. Once the doctor places the implant, the device uses a two-in-one approach to reduce the symptoms of congestion, nasal obstruction, and polyps. It does this by keeping the sinus cavity open while releasing the medication directly into sinus tissue.
The procedure to put this implant into place is simple. It can be performed in the office, and you can go home shortly after it is completed.
Your doctor will first numb your nose to help you stay comfortable. Through the nasal opening, the doctor will insert the implant into your ethmoid sinus. Once it is in place, you usually cannot feel it, so patients do not typically complain about long-term discomfort due to the implant.
The implant can remain in place for up to 90 days to keep your sinus open and to reduce symptoms of nasal congestion and obstruction. However, you can have it removed sooner at your doctor’s discretion.
Dupixent
Dupixent may be an option for patients with chronic rhinosinusitis with polyps that is poorly controlled with medications. Dupixent is a medicine that is injected just below the skin. It is typically given in the abdomen or thigh, but the back of the upper arm is also an acceptable injection site.
This medicine is classified as a biologic. It works to suppress and target the specific elements that trigger immune system inflammation. Injections are given every two weeks.
If intranasal steroids and other medications are not adequately controlling your nasal polyps and related symptoms, then Dupixent could be a viable alternative. It may also reduce the need for surgery to remove nasal polyps.

Pick one of our convenient locations
for your Nasal Polyps Treatment
