Thinking about septoplasty and wondering what recovery looks like day by day? If a crooked septum, chronic sinusitis, or sleep apnea has fueled breathing problems, a clear roadmap can calm nerves. Here’s a concise guide to early milestones and small wins that make healing feel manageable from your first night onward.
From early swelling and stuffiness to that first clear breath, we’ll outline what to expect, when to call your team, and how to support the recovery process. Use this day-by-day map to plan work, sleep, and activity—so each stage feels purposeful, predictable, and aligned with your goals for comfort and results.
About Septoplasty Surgery at Penn Medicine Becker ENT & Allergy
Breathing difficulties from a deviated septum can disrupt your life in many ways, but we’re here to help. The board-certified ENTs at Penn Medicine Becker ENT & Allergy offer this effective and permanent solution to their patients who are good candidates.
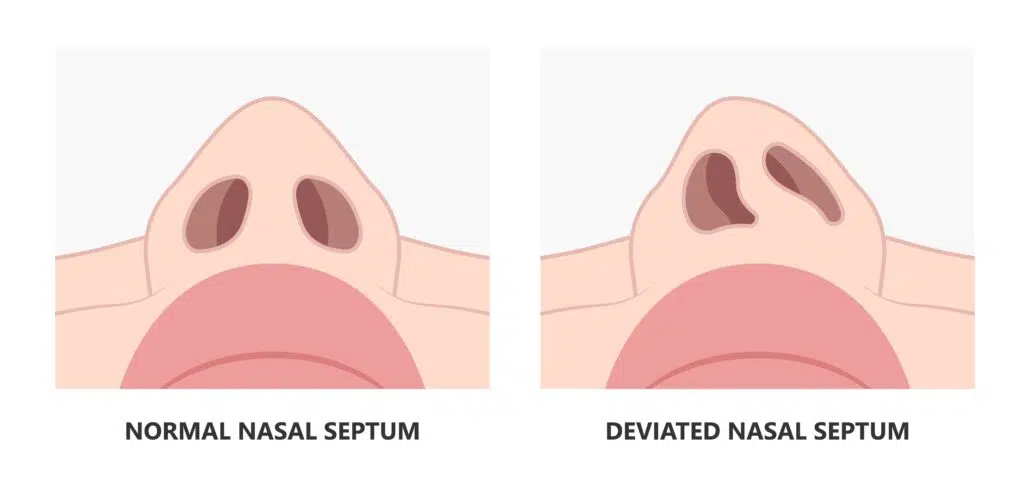
Septoplasty is a safe outpatient procedure, typically performed under general anesthesia. Through a small incision inside the nostril, the surgeon reshapes the deviated septum to improve airflow and relieve symptoms. In rare cases, the septum is removed, reconstructed, and re-implanted for the best possible results.
Day-by-day Septoplasty Recovery Timeline
Every recovery moves at its own pace, but most people pass through predictable stages. Use the outline below to track common milestones—what’s normal, what’s encouraging, and when to pause and call your team. Always follow your surgeon’s instructions if they differ; your operative details and overall health set the tempo.
First Few Days (0-3 Days)
Expect significant swelling, congestion, and mild to moderate discomfort during the first 72 hours. Light oozing or blood‑tinged drainage is common; wear a drip pad under the nose and change it whenever damp. Manage pain with your prescribed medication or acetaminophen only—avoid aspirin or ibuprofen, which can increase bleeding. Go home the same day, prioritize rest, and sleep with your head elevated to minimize swelling and pressure. Keep activity light at home. Choose cold, bland foods and frequent sips of water to stay hydrated; small, regular meals often feel easier. As drainage tapers, most people notice pressure easing.
First Few Days
First Week
Swelling and congestion crest early and begin to ease this week, though your nose will still feel blocked and tender. Many people feel well enough to return to desk work or school for shortened days, taking breaks to rest and hydrate. Gentle walking supports circulation and reduces stiffness, but avoid bending, heavy lifting, and any exercise that raises your heart rate significantly. You’ll likely have a follow‑up visit to remove splints or packing and to confirm healthy healing. Do not blow your nose; instead, use frequent saline sprays or rinses to keep tissues moist. Continue sleeping with your head elevated and keep meals soft.
First Week
Weeks 2-4
By weeks 2–4, swelling steadily recedes; congestion changes from pressure to dryness, and gentle saline rinses help. Breathing begins to feel easier as nasal tissues heal; airflow may fluctuate day to day. Most patients resume light daily routines and short walks; some return to light cardio like stationary cycling at low intensity if cleared. Avoid heavy lifting, high‑impact exercise, inversions, and contact sports. No nose blowing; sneeze with your mouth open. Continue sleeping slightly elevated if stuffy. If bruising or drainage worsens, call. Mild tenderness to touch and occasional crusting are normal—don’t pick. Keep follow‑ups and taper medications as directed.
Weeks 2-4
Weeks 4-6
By weeks 4–6, most swelling has settled and breathing is noticeably easier, though occasional dryness or morning stuffiness can linger. If your surgeon clears you, you may resume moderate exercise—brisk walking, easy cycling, or light strength work—while avoiding contact sports, high‑impact training, and heavy lifting. Keep saline rinses to maintain moisture and gently clear crusts; don’t pick inside the nose. Many people feel back to normal daily routines by the end of this period, but internal healing of bone and cartilage is still ongoing, so pace activities and protect your nose from bumps. If new fever, worsening pain, or thick discharge appear, call your team.
Weeks 4-6
Weeks 7 & Beyond
From about week 7 onward, most people see the day‑to‑day result they were hoping for—easier breathing and a quieter nose. Subtle refinement continues as internal tissues remodel over many months, so comfort and airflow can keep improving. You may return to full exercise and sports only when your surgeon clears you; protect your nose from bumps and use helmets or masks as advised. Keep gentle saline care until dryness fades, and avoid picking or forceful blowing. Manage allergies and colds promptly to limit swelling. Attend any recommended follow‑ups to confirm septal alignment. Call if you develop a fever, worsening pain, thick discharge, or new bleeding.
Weeks 7 & Beyond
Patient Testimonials
Tips for a Smooth Recovery from Septoplasty
Small, consistent habits add up. The tips below support an optimal healing process by minimizing swelling and bleeding risk, protecting the septum as tissues mend, and keeping you comfortable. Always follow your surgeon’s personalized instructions first; if guidance differs, their plan takes priority.

Good Incision Care
Keep the nostril/columella area clean and hands off. Change the drip pad as needed, but don’t press or wipe inside the nose. If you were given an ointment, apply a thin layer to the incision line as directed; otherwise, use saline spray/rinses to gently loosen crusts. Do not pick or use cotton swabs deep in the nose. Leave any splints or stitches completely alone until your follow‑up—no trimming or tugging. Pat dry after showers and avoid makeup or sunscreen on healing skin.

Don’t Blow Your Nose
Resist the urge to blow your nose, even if nasal congestion feels intense. Blowing can trigger bleeding, disrupt healing tissues, and dislodge clots. Instead, dab gently with a drip pad for any light drainage and let mucus exit passively. Use frequent saline nasal spray or rinses to humidify and mobilize secretions; sniffing should be gentle, not forceful. If you need to sneeze, open your mouth to release pressure. Call your care team if congestion suddenly worsens or you notice fresh bleeding.
Stay Well-Hydrated
Hydration supports circulation, reduces headaches, and thins secretions. Take steady sips of water throughout the day rather than large chugs, and pair fluids with light snacks if you feel queasy. Limit caffeine and skip alcohol early, as both can dehydrate and may raise bleeding risk. Broths, smoothies, and electrolyte drinks are useful if your appetite is low. Use saline sprays or rinses to keep nasal passages moist while you recover—dryness invites crusting. Aim for pale‑yellow urine; a darker color usually means you need more fluids.
Avoid Strenuous Activity
Plan plenty of rest for several days after surgery. Avoid heavy lifting, bending, high‑impact exercise, and any activity that raises heart rate or blood pressure. Short, frequent, gentle walk around the house or outside is encouraged—it improves blood flow, lowers stiffness, and helps prevent clots. Keep your head above your heart; no inversions, contact sports, or swimming. Resume gradual activity only with your surgeon’s clearance and stop if you notice throbbing, bleeding, or a jump in congestion.
Eat a Healthy Diet
Begin with cool, soft options the first few days—yogurt, applesauce, smoothies, scrambled eggs—then advance to balanced meals as appetite returns. Prioritize protein (fish, eggs, tofu, beans) to support tissue repair, plus colorful fruits and vegetables rich in vitamin C. Choose whole grains and fiber to counter constipation from pain medicines. Keep sodium modest to help limit fluid retention and swelling. Avoid very hot or spicy foods early, which can increase nasal blood flow. Small, frequent meals and gentle snacks often feel best.
Avoid Alcohol and Nicotine
Skip alcohol until your surgeon clears you. It dilates blood vessels, raises bleeding risk, interacts with pain medicines, and dehydrates—none of which helps early healing. Avoid nicotine in all forms (cigarettes, vaping, pouches, cigars); it constricts blood flow, lowers oxygen to tissues, and slows repair, increasing infection and scarring risk. Steer clear of secondhand smoke, too. If quitting is hard, ask your care team about safe, temporary supports; some nicotine replacements still constrict vessels, so get guidance before using them.
Sneeze Through the Mouth
When a sneeze builds, open your mouth so most of the force exits forward rather than through the nose. Don’t pinch your nostrils or stifle the sneeze—back‑pressure can disturb healing tissues and raise bleeding risk. Turn your head, cover with a tissue, and let it out gently. If allergies trigger sneezing, use surgeon‑approved antihistamines and regular saline to calm irritation. Keep indoor air humidified and avoid smoke or dust. Call your care team if sneezing is frequent or brings fresh bleeding.
Follow Post-Op Instructions
Your discharge sheet is your playbook—follow it exactly. Take medications at the prescribed times; unless specifically instructed by your doctor, take your medicine after meals to reduce nausea. Use saline sprays/rinses as scheduled and don’t add over‑the‑counter products without approval. If your team approves, apply a cold pack on your nose for 10 to 20 minutes at a time, with a cloth barrier, then remove for an equal time. Keep head elevated, attend follow‑ups, and call for fever, worsening pain, thick discharge, or brisk bleeding.
Why Schedule a Septoplasty with Dr. Daniel G. Becker
Who Should Perform My Septoplasty Surgery?
Choosing an experienced septoplasty team matters: subtle decisions during surgery influence swelling, scarring, airflow, and long‑term comfort. A seasoned ENT and nasal surgery specialist understands how to protect delicate structures, optimize function, and guide safe activity progression—helping you heal efficiently and reduce complications on the path to lasting, natural breathing.
At Penn Medicine Becker ENT & Allergy, your septoplasty is performed by a fellowship‑trained surgeon within a multidisciplinary center—otolaryngologists, facial plastic surgeons, allergists, audiologists, and speech‑language pathologists—using advanced techniques and technology.
Our physicians have published extensively, lecture internationally, and hold patents for innovative instruments. Ready to breathe easier? Visit our contact page to schedule a consultation, or head to our Locations page to find the phone number for your city.

