Recovery after sinus surgery takes time and involves a few key steps to help the body heal properly. Taking the right approach early on can prevent complications and lead to a smoother experience.
Most people want to know how to care for themselves after surgery, how long recovery will take, and what they can do to feel better faster. At Penn Medicine Becker ENT & Allergy, our sinus experts offer trusted care and clear advice to support every stage of your recovery.

What to Know Before and After Sinus Surgery
- Sinus surgery helps relieve chronic sinus problems when other treatments haven’t worked.
- Before sinus surgery, following your doctor’s instructions and planning for recovery makes a big difference.
- After sinus surgery, resting, avoiding heavy activity, and eating well can speed up healing.
- Keeping your nose clean and moist after sinus surgery helps prevent irritation and supports recovery.
- Pain after sinus surgery is common, but your doctor can recommend ways to manage it safely.
How Can I Prepare for Sinus Surgery?
Proper preparation is crucial for successful sinus surgery and recovery. Here are some steps to follow before your surgery:
What Are the Best Recovery Tips After Sinus Surgery?
Following your sinus surgery, it is essential to adhere to your doctor’s recommendations and take steps to ensure a smooth recovery time and faster healing. Here are some tips to help you during the post-surgery period:
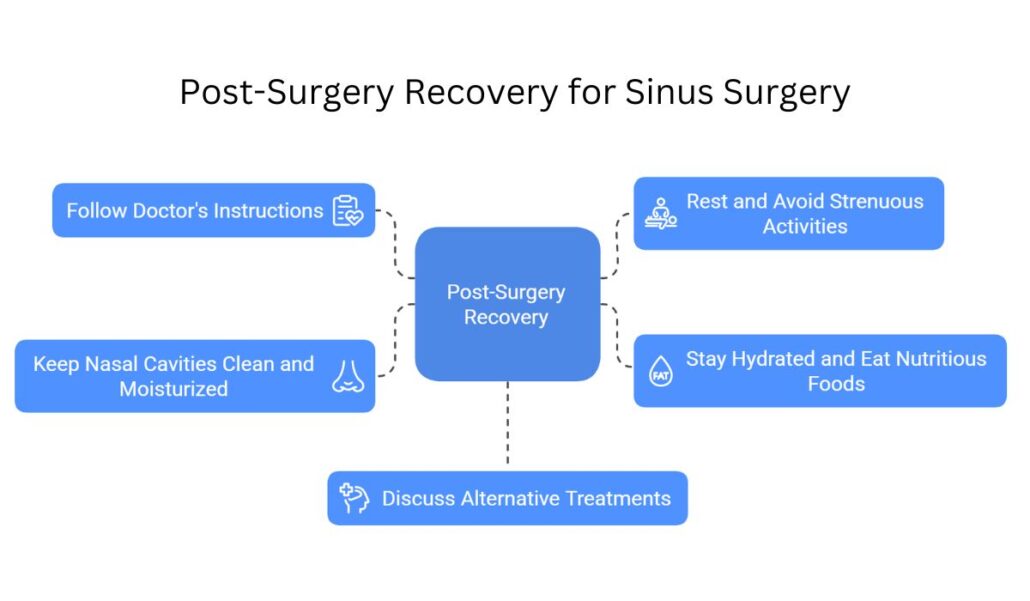
Take Time to Rest and Recover
Plenty of rest is crucial for a successful sinus surgery recovery. Ensure that you get plenty of sleep and avoid overexerting yourself. Elevate your head while resting to help minimize swelling and promote sinus drainage. Additionally, avoid bending over or lifting heavy objects, as this can increase pressure in your sinus passages and cause discomfort.
Avoid Strenuous Activities
For at least two weeks after surgery, avoid engaging in strenuous activities, such as vigorous exercise, sports, or heavy lifting. These activities can increase blood pressure and cause bleeding or other complications. Consult with your doctor before resuming any physical activities to ensure your sinuses have adequately healed.
Follow Your Doctor’s Instructions
Your doctor will provide you with specific post-surgery care instructions, such as how to clean your nasal passages and when to schedule follow-up appointments. It is essential to follow these instructions closely to ensure a successful recovery and prevent complications. Always take doctor-prescribed antibiotics as directed. If you have any questions or concerns, do not hesitate to contact your doctor for guidance.
Stay Hydrated and Eat Nutritious Foods
Maintaining proper hydration and nutrition is vital for a proper healing process. Drink plenty of water and consume a well-balanced diet rich in fruits, vegetables, and lean proteins. Avoid consuming spicy foods, as they can cause irritation and discomfort in your nasal passages.
Keep the Nasal Cavities Clean and Moisturized
Keeping your nasal passages clean and moisturized is essential for promoting healing and preventing infection. Use a saline nasal spray as directed by your doctor to help keep your nasal passages moist and clean. Additionally, using a humidifier in your home can help maintain proper humidity levels and prevent dryness in your nasal passages.
Talk to Your Doctor About Alternative Treatments
In some cases, additional treatments may be necessary to address ongoing sinus issues or complications following surgery. It is essential to communicate with your doctor regularly about any persistent symptoms or concerns you may have. They may recommend alternative treatments, such as allergy medications, nasal corticosteroids, or additional surgical procedures to address your specific needs.
Managing Pain After Sinus Surgery

Pain management is an essential aspect of recovery after sinus surgery. Your doctor will likely prescribe pain medication to help manage any discomfort you may experience following the surgery. Be sure to follow the medication instructions as directed and do not exceed the recommended dosage.
Over-the-counter pain relievers, such as acetaminophen or ibuprofen, may also be recommended to help manage pain. However, always consult with your doctor before taking any over-the-counter medications to ensure they are safe and appropriate for your specific situation.
Get the Support You Need for a Smooth Sinus Surgery Recovery
Take the stress out of healing—our experienced team is here to guide you every step of the way.
Regaining Normal Activities After Sinus Surgery
You can usually return to your normal activities within one to two weeks after sinus surgery, as long as your healing is going well and your doctor gives you the go-ahead.
Recovery timelines can vary, but most people start feeling better within a few days and gradually ease back into work, school, and daily routines. The key is to take it slow and not rush things—your body needs time to heal. Even if you start to feel good quickly, pushing yourself too hard can set back your recovery.
Your doctor will guide you on what’s safe based on the type of surgery you had and how you’re healing. Some things, like heavy lifting, strenuous exercise, or flying, might need to wait a bit longer. It’s important to follow your post-op instructions and check in with your doctor if you’re unsure about doing something.
Listen to your body. If you feel tired or uncomfortable, that’s your signal to rest. Taking care of yourself during this time helps you get back to feeling your best sooner.

What Are the Possible Risks or Complications After Sinus Surgery?
While sinus surgery is generally considered safe and effective, there are potential complications that can arise. Some possible complications include infection, bleeding, scarring, and a change in sense of smell or taste. It is essential to be aware of these potential risks and to closely follow your doctor’s post-surgery care instructions to minimize the likelihood of complications. If you experience any unusual symptoms or have concerns about your recovery, do not hesitate to contact an ENT specialist.
Get an Appointment with a Sinus Expert in NJ & PA
If you are considering sinus surgery and want to ensure a successful recovery, Penn Medicine Becker ENT & Allergy is the place for you. Our experienced staff provides comprehensive care to help you properly prepare for surgery and manage the pain afterward. From providing vital information about the procedure to offering alternative treatments, we are here to support your journey from beginning to end. Contact us today and take one step closer to a successful sinus surgery recovery.