Latex allergy is a common health problem that can have mild to serious effects on people who are sensitive. Latex is a milky liquid that comes from plants or trees that are laticiferous. It is used in many medical and consumer goods because it forms a strong, flexible shield that water can’t get through.
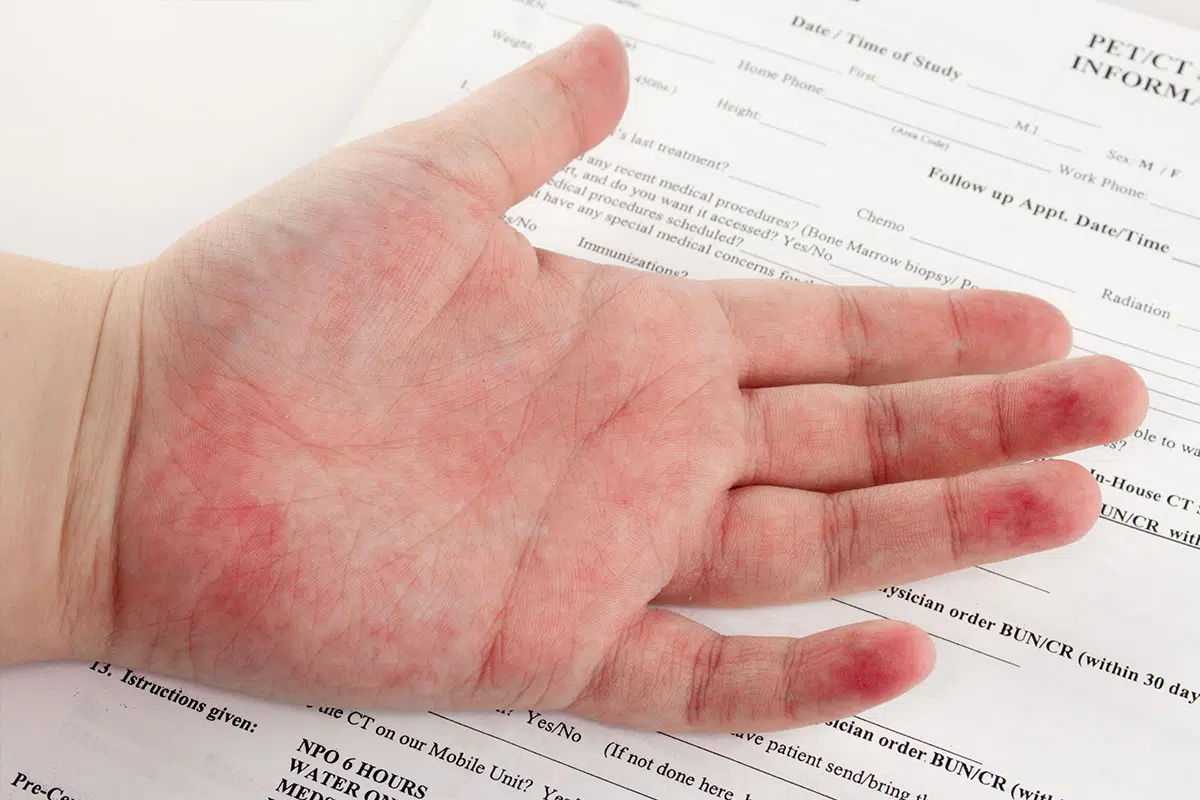
People who are allergic to latex often have skin responses like hives and itching, breathing problems like wheezing, or in the worst cases, anaphylaxis. Most of the time, the allergy is caused by direct contact with latex goods, such as gloves and medical devices. However, it can also be caused by breathing in latex particles or eating foods that are cross-reactive.
Understanding the importance of latex allergy tests, the various types of tests available, and how to prepare for them is crucial for individuals who are at risk.
Importance and Benefits of Latex Allergy Tests
Diagnosing and controlling latex allergies as well as avoiding anaphylactic risk, chronic skin irritation, and respiratory issues depend on latex allergy tests. While anaphylaxis is the most extreme, immediate allergic reactions to latex can be rather severe.
These tests are especially helpful for people who have had allergies in the past, healthcare workers, and people who come into regular touch with latex products like medical devices, rubber gloves, and elastic bands. These groups are more likely to be allergic to latex because they are exposed to it more often.
Different Types of Latex Allergy Tests
There are two main types of latex allergy tests: skin prick tests and blood tests.
A skin prick test puts a small amount of latex protein on the patient’s skin and watches to see if they have any bad responses. Most of the time, an allergist does this test to establish a diagnosis of latex allergy.
A blood test, on the other hand, is used to detect the presence of latex IgE antibodies in the blood. A positive blood test suggests a latex allergy, but it does not confirm the diagnosis.
Both the clinical history and identification of latex-specific IgE antibodies are needed to confirm latex allergy. It’s important to note that irritant dermatitis may occur before a person develops a latex allergy. A person can also have both irritant dermatitis and a latex allergy at the same time. This is why comprehensive testing is crucial to ensuring accurate diagnosis and treatment.
Preparing for a Latex Allergy Test
Before undergoing a latex allergy test, it’s crucial to follow certain guidelines to ensure accurate results. Firstly, you should avoid potential allergens prior to the test.
This includes minimizing contact with latex products like gloves, balloons, and certain medical devices. In addition, it’s important to inform your healthcare provider about any medications or substances you are currently taking, as they may interfere with the test results.
Certain medications, such as antihistamines or steroids, can affect skin tests and should be discontinued several days before testing under the guidance of a healthcare provider.
The Procedure and Process of Latex Allergy Testing
The procedure for a skin prick test involves observing for allergic reactions like redness or swelling after applying a small amount of latex protein to the skin.
The process of a blood test involves taking a small blood sample to measure latex-specific IgE antibodies.
This test is useful for those who can’t undergo skin testing due to severe conditions like atopic dermatitis or the risk of an anaphylactic reaction.
These tests can indicate sensitivity to natural rubber latex, but they do not diagnose a latex allergy. A positive test means the immune system has produced antibodies to latex, but it doesn’t mean the person will show allergy symptoms when exposed to latex products.
Interpreting and Understanding the Test Results
Interpreting the outcomes of a latex allergy test can be intricate and is best performed by an expert allergist.
In the case of skin prick tests, a positive reaction is usually signified by a raised, red bump on the skin, akin to a mosquito bite, at the site of the test. The size of this bump can offer insights into the intensity of the allergy.
In blood tests, the detection of latex-specific IgE antibodies in the blood implies an allergy to latex.
The quantity of these antibodies does not always align with the severity of the allergic reactions. Some individuals with high levels of latex-specific IgE antibodies might only exhibit mild allergic symptoms, while others with lower levels might experience severe reactions. In both testing methods, a negative outcome typically suggests that the person does not have a latex allergy.
However, no test is infallible, and there is a possibility of false-negative or false-positive results. Consequently, the results of the test should always be evaluated in relation to the person’s clinical history and symptoms.
Secure Your Safe Treatment Experience with PennMedicine
Join our satisfied clients who’ve experienced safe, effective treatments.
Developing an Action Plan Based on Test Results
After your latex allergy test:
Create an action plan with your allergist, considering your allergic reactions, lifestyle, and job.
If diagnosed with a latex allergy, avoid latex-containing products and use alternatives like synthetic rubber products or polyvinyl chloride items.
Inform your doctor, employer, and family about your allergy.
If you work in high-risk areas like healthcare, request non-latex gloves. If accidentally exposed to latex, use medications like antihistamines or corticosteroids to manage the allergic reaction. For severe reactions, have an epinephrine auto-injector and seek immediate medical help. Individuals with a latex allergy should wear a medical alert bracelet and carry a card detailing their allergy for emergencies.
Conclusion and Final Thoughts on Latex Allergy Tests
Latex allergies, particularly those caused by natural rubber latex, can lead to a range of reactions, from irritant contact dermatitis and allergic contact dermatitis to severe reactions such as anaphylactic shock. These reactions can occur upon direct contact with latex products or through exposure to airborne latex particles.
Given the widespread use of latex in medical devices, from rubber gloves to urinary catheters, and the high rate of latex allergy among healthcare workers, early detection and management of this allergy is of utmost importance. Skin prick tests and blood tests are the primary testing methods for diagnosing latex allergies.
These tests measure the presence of latex-specific IgE antibodies in the body, which are indicative of an allergic reaction to latex. However, it’s essential to interpret these results in the context of the individual’s medical history and clinical manifestations of the allergy. For instance, common symptoms such as itchy skin, skin rash, runny nose, and chest pain should be considered alongside test results.
People with a history of allergies, particularly food allergies, or who have a family history of latex allergies are at a higher risk and should consider undergoing testing.
To learn more about latex allergy tests and how to manage your latex allergy, contact Penn Medicine Becker ENT & Allergy to request an appointment with an expert allergist.

